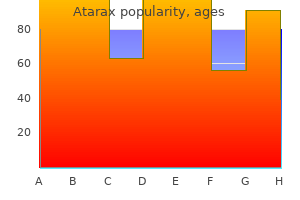
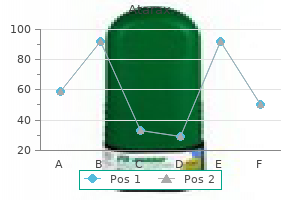
Atarax
Atarax
Atarax dosages: 25 mg, 10 mg
Atarax packs: 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills
We put together a syringe of 3% 2-chloroprocaine to be used if emergency extension of epidural anesthesia is required anxiety 05 mg atarax 10 mg cheap online, and we even have nitroglycerin immediately obtainable in case uterine rest is required acutely for supply of twin B anxiety symptoms knee pain atarax 25 mg visa. At least one member of the anesthesia staff stays with the affected person till twin A is delivered and twin B is either delivered or the vertex is well applied within the pelvis symptoms 0f anxiety atarax 25 mg best. An analgesic spinal dose can be administered for the second stage of labor and vaginal supply, whereas the epidural catheter can be utilized to prolong the block if cesarean delivery is required. Vaginal Delivery of Twin A/Operative Delivery of Twin B the flexibility related to epidural analgesia is especially advantageous if the obstetrician delivers twin A vaginally but twin B requires operative supply. We administer a Twin B If twin A is delivered vaginally, the obstetrician must make a decision concerning the methodology of delivery of dual B. Presentation and place should be verified, because these can change after delivery of twin A. If twin B has a vertex presentation and the pinnacle is nicely applied to the cervix, or if the amniotic membranes are still intact in a diamniotic being pregnant, the obstetrician may enable the affected person to resume labor and await spontaneous vaginal delivery. Mothers who received epidural anesthesia shall be extra relaxed and will tolerate the procedure higher than these with out neuraxial anesthesia. Total breech extraction is taken into account applicable if twin A is similar size or larger than twin B to ensure that the pelvis and cervical dilation are enough for vaginal supply of twin B, and if supply is attempted early after supply of twin A to be sure that the cervix has not begun to contract. In the previous, obstetricians favored the delivery of twin B within 15 to 30 minutes of delivery of twin A. Once the obstetrician determines that cesarean delivery will be necessary, we inject extra local anesthetic to lengthen the surgical sensory degree to approximately T4 utilizing 3% 2-chloroprocaine for fastest onset. Pain aid and skeletal muscle leisure (both supplied by epidural anesthesia) facilitate internal model and whole breech extraction of dual B. In some cases, pharmacologic uterine relaxation may be required to facilitate inner version and breech extraction of twin B. Sublingual (400 �g) or intravenous (150 to 250 �g) administration of nitroglycerin ought to present enough relaxation for inside podalic version. If this maneuver is unsuccessful, rapid-sequence induction of basic anesthesia, adopted by administration of a excessive focus of a risky halogenated agent could additionally be wanted. Cesarean Delivery Epidural, spinal, or basic anesthesia can be safely administered for elective abdominal supply. A historical desire for epidural anesthesia was based on the gradual onset of sympathetic blockade, which was thought to reduce the incidence of extreme hypotension. It has been long believed that ladies with multiple gestation are at higher threat for hemodynamic instability during administration of neuraxial anesthesia than girls with a singleton gestation. Comparison of brachial artery (arm) and popliteal artery (leg) blood pressures may allow the detection of occult supine hypotension, which results in reduced uteroplacental perfusion in the presence of a normal brachial artery pressure. If both hypotension or occult supine hypotension is detected or suspected, further left uterine displacement or displacement to the opposite facet might resolve the problem. A mixed spinal-epidural anesthetic permits the anesthesiologist to use a lower dose of spinal anesthetic if desired, while retaining the aptitude of raising the anesthetic level using epidural local anesthetic if needed. Vallejo and Ramanathan90 demonstrated that imply umbilical venous and umbilical arterial lidocaine concentrations were 35% to 53% greater in twin newborns than in singleton newborns uncovered to epidural anesthesia for cesarean delivery. Mean fetal-to-maternal lidocaine ratios were at least 18% larger within the twin newborns than in the singleton newborns. The investigators speculated that this distinction could also be a result of larger maternal cardiac output and plasma volume associated with twin gestation in addition to the decreased total plasma protein concentration, which results in a rise in the free lidocaine concentration. When common anesthesia is used, higher oxygen consumption and decreased practical residual capability related to a quantity of gestation will increase the risk for maternal hypoxemia during times of apnea. The presence of two or extra fetuses ends in a protracted uterine incision-to-delivery interval due to the longer time required to ship multiple infants. A extended interval increases the danger for umbilical wire blood acidemia and neonatal depression. Neonatal despair, especially of twin B, is less likely with neuraxial anesthesia than with general anesthesia. Successful external cephalic version helps reduce the risk for perinatal morbidity and mortality related to breech supply and lowers the cesarean supply rate. Neuraxial anesthesia may enhance the success price of exterior cephalic model, including after an preliminary failed attempt. Specifically, it (1) supplies effective pain reduction; (2) inhibits early pushing; (3) relaxes the pelvic flooring and perineum, facilitating atraumatic supply of the aftercoming head; and (4) allows provision of anesthesia for emergency cesarean delivery. Provision of ache relief and skeletal muscle leisure facilitates the vaginal supply of twin B. Provision of epidural analgesia also facilitates the administration of anesthesia for emergency cesarean delivery whether it is needed. Intravenous or sublingual nitroglycerin offers fast uterine relaxation of brief period. Alternatively, rapid-sequence induction of general anesthesia followed by administration of a excessive focus of a risky halogenated agent is one other dependable methodology of providing uterine and cervical leisure. Sonographic analysis of the fetal backbone position and success fee of manual rotation of the fetus in occiput posterior place: a randomized controlled trial. Manual rotation to reduce caesarean delivery in persistent occiput posterior or transverse place. Planned caesarean part versus deliberate vaginal birth for breech presentation at term: a randomised multicentre trial. Mode of supply after profitable external cephalic model: a scientific review and meta-analysis. Maternal outcomes at 2 years after planned cesarean section versus deliberate vaginal start for breech presentation at term: the worldwide randomized time period breech trial. Maternal and neonatal outcome of 846 time period singleton breech deliveries: seven-year experience at a single middle. Clinical factors to predict the end result of external cephalic model: a metaanalysis. Contraindications for external cephalic model in breech place at time period: a scientific evaluation. A randomized placebo-controlled evaluation of terbutaline for exterior cephalic version. Intravenous nitroglycerin for exterior cephalic version: a randomized managed trial. Interventions for serving to to turn time period breech babies to head first presentation when using external cephalic model. External cephalic version for breech presentation with or with out spinal analgesia in nulliparous ladies at term: a randomized managed trial. Randomized managed trial of external cephalic version in term multipara with or with out spinal analgesia. Atrial natriuretic peptide, blood volume, aldosterone, and sodium excretion throughout twin pregnancy. A randomized trial of amnioreduction versus septostomy within the therapy of twin-twin transfusion syndrome. Operative fetoscopy in difficult monochorionic twins: present standing and future direction. Pregnancy outcome in spontaneous twins versus twins who had been conceived via in vitro fertilization. Co-twin prognosis after single fetal dying: a systematic review and meta-analysis. Maternal morbidity and toddler death in twin vs triplet and quadruplet pregnancies. Randomized trial of anaesthetic interventions in external cephalic version for breech presentation. Effect of intrathecal bupivacaine dose on the success of exterior cephalic version for breech presentation. Outcomes at 3 months after deliberate cesarean vs planned vaginal delivery for breech presentation at term: the worldwide randomized term breech trial. Once more into the breech: deliberate vaginal supply in contrast with planned cesarean supply. Determinants of perinatal mortality and serious neonatal morbidity within the second twin. The anesthetic administration of triplet cesarean supply: a retrospective case sequence of maternal outcomes. Severe acute maternal morbidity in a quantity of pregnancies: a nationwide cohort study.
Diseases
Obstetric and anesthesia providers can expect to encounter a growing number of pregnant ladies with surgically-closed open spinal dysraphisms anxiety quotes bible order atarax 25 mg fast delivery. Many patients have significant residual neurologic impairment and ongoing orthopedic and genitourinary complications anxiety medication side effects discount atarax 25 mg on line. Hydrocephalus is present in many sufferers anxiety 24 weeks pregnant atarax 10 mg order with amex, and shunting of the ventricular system is widespread, with revisions typically required throughout childhood. Closed spinal dysraphisms are further divided into those with or without a subcutaneous mass. The lesions are normally in the lumbosacral area, and the skin overlaying these defects is frequently irregular. Dermal sinus tracts ought to to not be confused with pilonidal cysts; dermal cysts are frequently linked to the intradural space and therefore pose a threat for creating meningitis. A new classification of tethered cord syndrome in adults has been proposed to differentiate tethered cord occurring secondary to open spinal dysraphism from the adult-onset neurologic syndrome related to closed spinal dysraphism. Tethered twine from a tight filum terminale has additionally been deemed causal within the improvement of syringomyelia and subsequent Arnold-Chiari syndrome. The white arrow signifies the termination of the conus medullaris at L4 to L5, and the black arrow indicates the filum terminale situated at L5 to S1. Cesarean delivery is reserved for obstetric indications, and its incidence is increased and proportionate to the severity of the underlying defect and its consequences. Pelvic and lower limb anomalies and contractures might impede the pelvic outlet and warrant cesarean supply. Cesarean delivery is difficult by the presence of stomas and conduits; postoperative problems and prolonged hospital stays are frequent. Anesthetic Management Administration of epidural or spinal anesthesia could also be thought-about in ladies with various types of spinal dysraphism and steady neurologic operate. Imaging studies provide priceless data on neural anatomy and facilitate anesthetic administration. An isolated laminar arch defect rarely causes points for administration of neuraxial anesthesia. First, the lesion typically occurs at the L5 to S1 segments, beneath the level at which most epidural and spinal anesthetics are administered. Second, the most common anomaly is an easy midline cut up within the lamina, and this defect not often appears to interfere with either the efficiency or the development of spinal or epidural anesthesia. The epidural area could additionally be incomplete or discontinuous throughout the level of an isolated laminar arch defect due to the variable formation of the ligamentum flavum at this web site. An try to determine the epidural house at the website of this lesion may end in unintentional dural puncture, although successful epidural analgesia has been reported with the catheter placed throughout the zone of the lesion. If spinal dysraphism is suspected however no imaging research can be found, it could be prudent to keep away from neuraxial anesthesia. In the patient with an open spinal dysraphism lesion, the anesthesia provider ought to decide the extent of the lesion and whether or not the affected person has residual spinal wire operate beneath it. Patients with a complete lesion at or above T11 are more probably to experience painless labor. However, the risk for autonomic hyperreflexia ought to be evaluated in patients with thoracic lesions, and neuraxial anesthesia ought to be offered if the affected person is deemed to be at risk; this concern is particularly important if the lesion is between T5 and T8 (see Chapter 48). If the affected person has undergone ventricular shunt placement, the current status of the shunt should be decided. Neurosurgical consultation ought to be obtained if questions remain about the requirement for, or perform of, the shunt. Baseline renal operate should be assessed as nicely as pulmonary operate, especially in sufferers with scoliosis. There are published reviews of the use of epidural and spinal anesthesia in sufferers with open spinal dysraphism. Tidmarsh and May102 reported the administration of intrapartum analgesia in sixteen patients with spinal dysraphism, eight of whom had myelomeningocele. Five of the eight patients with open spinal dysraphism received epidural analgesia for labor and delivery. Three patients had a "normal" block, one affected person had a sensory stage that was higher than anticipated (T3 after the administration of 10 mL of 0. There had been quite a few complications ranging from troublesome block placement; speedy onset of anesthesia; and uneven, high, and failed blocks, certainly at a price far larger than in typical obstetric patients. If attainable, epidural analgesia should also be initiated below the level of twine termination in case of unintentional dural puncture. It ought to be famous that the epidural area is commonly abnormal, which will increase the likelihood of inadequate epidural anesthesia. Limited information exist on the obstetric anesthesia expertise in parturients with Arnold-Chiari malformation. Nine deliveries have been accomplished with neuraxial anesthesia, including six vaginal deliveries with epidural analgesia, two cesarean deliveries carried out with single-shot spinal anesthesia, and one cesarean supply carried out with a spinal catheter. No affected person experienced postprocedural neurologic sequelae associated to the usage of neuraxial anesthesia. There is considerable interindividual variation in the medical and radiographic traits, and skeletal abnormalities usually present more variation than consistency. Anesthetic drug-dosing, mechanical air flow methods, and postdelivery pain administration need to be thought-about fastidiously as the disproportion between truncal dimension and limb measurement could lead to errors. The illness is a generalized connective tissue dysfunction, and expression ranges from mild osteoporosis to the classical clinical stigmata characterized by a number of bone fractures and skeletal deformities, blue sclera, and center ear deafness (otosclerosis). There are now eight sorts categorized by genetic mutations, although scientific features are still the first differentiation. It is inherited as an autosomal dominant trait and is the most common and mildest type of this illness. Back discomfort is frequent throughout pregnancy, and the reported incidence of sciatica is bigger than in wholesome pregnant ladies,112 more than likely owing to the underlying spinal abnormalities. Typically, an inadequate maternal pelvis combined with a normal-sized (nonachondroplastic) fetus leads to cephalopelvic disproportion. Imaging techniques could also be used to confirm this example, and the obstetrician ought to anticipate the need to deliver most sufferers with achondroplasia by cesarean delivery. Prominent paraspinal muscles and marked lumbar lordosis may complicate makes an attempt to palpate landmarks in the course of the administration of spinal or epidural anesthesia; the use of ultrasonography may help determine landmarks. The small stature and spinal stenosis scale back the dose of native anesthetic required for major neuraxial anesthesia. Generalized osteoporosis, corrected thoracic kyphoscoliosis, a restricted thoracic cage, and multiple old fractures are demonstrated. Transfers, positioning, and any invasive intervention have to be achieved with excessive care. Blood stress cuffs and tourniquets to facilitate placement of intravenous catheters ought to be utilized gently to forestall fractures. Alternatives to direct laryngoscopy, such as video laryngoscopy, could additionally be thought of to reduce the applied forces needed for direct laryngoscopy. Authors of a case report raised the theoretical concern that fasciculations following succinylcholine administration could also be harmful. The possibility of platelet dysfunction is best evaluated by acquiring a thorough bleeding history. Small stature and spinal abnormalities cut back the native anesthetic dose requirements and enhance the risk for each misplaced injection and local anesthetic systemic toxicity. It may be difficult to estimate the suitable dose for single-shot spinal anesthesia in these sufferers. Dwarfism is typical, and kyphoscoliosis is common, as are different chest wall abnormalities. Other abnormalities embody a decrease within the vary of movement of the shortened cervical spine, micrognathia, and malformed, brittle teeth. Hyperthyroidism occurs in 40% of patients; an elevated concentration of thyroxine results in increases in each oxygen consumption and warmth production. Obstetric Management Pregnancy leads to transfer of calcium from the mom to the fetus, which in the patient with osteogenesis imperfecta can lead to elevated maternal fracture threat. Prepregnancy pulmonary perform is a better predictor of maternal end result than the severity of the curve. Association between lumbopelvic ache, incapacity and sick leave throughout pregnancy - a comparability of three Scandinavian cohorts.
Echocardiography helps predict overall cardiac danger and guides anesthetic management in pregnant ladies with cardiac illness anxiety symptoms from work buy 25 mg atarax with amex. Contemporary proof suggests that for commonest cardiac circumstances anxiety symptoms go away purchase atarax 10 mg with visa, handheld transthoracic echocardiography supplies extra correct prognosis than physical examination anxiety hives atarax 10 mg for sale. Echocardiographic measurements of cardiac output improve during being pregnant owing to will increase in stroke quantity and coronary heart fee. Importantly, stroke work is elevated throughout being pregnant, which is in preserving with augmented myocardial fiber perform. Both the best and left ventricular chamber dimension are elevated in end-diastole and end-systole, and the guts becomes more globular. This improve in chamber dimension ends in elevated left ventricular end-systolic and end-diastolic volumes and is accompanied by an increase in left ventricular wall thickness (eccentric left ventricular hypertrophy). Combined with a small additional enhance in coronary heart price, this alteration ends in a 20% greater increase in maternal cardiac output with a quantity of gestation compared with singleton gestation. In regular pregnancy, left ventricular diastolic operate is elevated in the first two trimesters and declines within the third trimester. Additionally, through the process, the left lateral decubitus place could be extra simply maintained with radial access. The use of pulmonary artery catheterization has significantly declined in the United States in latest years. Similar info may be obtained noninvasively by transthoracic or transesophageal echocardiography. However, thermodilution and Fick cardiac output measurements could be obtained only with using a pulmonary artery catheter. Similarly, right-sided coronary heart catheterization is required for vasoreactivity testing in sufferers with pulmonary hypertension. Iodinated Contrast Use throughout Pregnancy the use of iodinated contrast media in pregnant ladies seems secure. Free iodide in the distinction medium administered to the mom could depress fetal, and subsequently neonatal, thyroid perform. Therefore, it has been suggested that neonatal thyroid operate be checked in the course of the first week postpartum. The slight potential danger associated with absorption of distinction medium is thought to be inadequate to suggest interruption of breast-feeding after maternal administration of iodinated distinction media. Thus, in being pregnant, invasive coronary angiography appears preferable beneath most circumstances. Gadolinium crosses the placenta and has been discovered to be teratogenic in animal models. Currently available human knowledge counsel that gadolinium must be used in pregnant girls provided that it considerably improves diagnostic performance and is predicted to improve maternal or neonatal consequence. Nonetheless, the most secure method is to keep away from ionizing radiation throughout being pregnant if potential, and to assess each the maternal and fetal dangers and advantages before deciding on essentially the most acceptable imaging modality. Other Drugs Hydralazine is used in the therapy of cardiomyopathy and can additionally be an excellent antihypertensive agent. Nitrates likely may be safely used long run in pregnant women with cardiomyopathy. Digoxin freely crosses the placenta, however its use has not been associated with congenital abnormalities or untoward fetal results. The widespread use of statins (which are related to exceptionally robust cardiovascular end result data) has remodeled the therapy of coronary artery illness. Nonetheless, given the critical significance of ldl cholesterol synthesis in the normal improvement of the embryo and placenta, and thus their potential for teratogenicity, statins are contraindicated in being pregnant. Longterm use could end in a discount in uteroplacental perfusion, which may be related to fetal development restriction and oligohydramnios. These medicine are significantly useful in nonpregnant sufferers with diabetes mellitus. These medicine cause fetal kidney malfunction and decreased fetal urine output, which leads to oligohydramnios. Prolonged and highdose use of these medication has been related to fetal growth restriction; however, the general risk is in all probability going small. Estrogen-induced changes in collagen deposition, as well as circulating elastases and relaxin, may weaken the aortic media and thus predispose the aorta to dissection throughout pregnancy. Approximately onehalf of aortic dissections and ruptures in women youthful than forty years of age are associated with pregnancy. Both medication appear to be safe and efficient therapies for cardiac arrhythmias in the second and third trimesters. Conditions that predispose girls to aortic dissection during pregnancy embrace Marfan syndrome, Ehlers-Danlos syndrome, bicuspid aortic valve,49 Turner syndrome, and non�Marfan syndrome�associated familial thoracic aneurysms. It has been hypothesized that contraction of the uterus causes outflow resistance, thus predisposing to aortic dissection after supply. In addition to brief stature, webbed neck, and characteristic facial features, Turner syndrome is associated with aortic coarctation and hypertension. Because of brief stature in some patients with Turner syndrome, absolute aortic root measurements may not precisely predict the risk for aortic dissection. Sporadic mutations are seen in roughly 25% of sufferers with no household history of this syndrome. Aortic dilation and aortic dissection contribute significantly to cardiovascular issues in these sufferers. Aortic dissection has been noticed during pregnancy and within the peripartum interval. In addition, visceral and iliac aneurysms, arterial tortuosity, and early-onset joint abnormalities may be present. In a cohort of 17 patients and 34 pregnancies, no maternal mortality or aortic dissection was observed. Cesarean supply was performed for mainly obstetric indications with out increased bleeding issues. Current tips are primarily based on professional opinion, case reviews, and present standard of care (level C evidence) (Box forty one. All recommendations are Level of Evidence C (very limited populations have been evaluated, and suggestions are based on consensus opinion of consultants, case research, or standard of care). Not occasionally, girls with an atrial septal defect might turn into symptomatic during being pregnant. The most common defect is the secundum-type atrial septal defect (80%), whereas the primum, sinus venosus, and coronary sinus types of atrial septal defect are much less widespread. Right ventricular overload results in pulmonary hypertension and Eisenmenger syndrome in lower than 5% of patients with an atrial septal defect. Cardiac problems are similar in women with unrepaired and repaired atrial septal defects. Preeclampsia, fetal demise, and small-for-gestational-age infants are extra widespread in pregnant ladies with an unrepaired atrial septal defect than within the basic obstetric population. Both neuraxial and basic anesthesia are acceptable for patients with a repaired or unrepaired atrial septal defect. Ventricular Septal Defect There are four kinds of ventricular septal defects; the commonest sort is a perimembranous ventricular septal defect. Pregnancy is nicely tolerated in women with a repaired ventricular septal defect or a small ventricular septal defect in the absence of pulmonary hypertension. An unrepaired ventricular septal defect with Eisenmenger syndrome is associated with a excessive danger for maternal cardiac complications (see later discussion). If the dissection happens in the third trimester and the fetus is deemed viable, an urgent cesarean supply adopted by aortic surgery may be performed. Both neuraxial63,64 and general anesthesia65 may be safely carried out in these patients, with emphasis on meticulous blood pressure stability and management. Invasive blood stress monitoring is really helpful to facilitate tight hemodynamic control. Dural ectasia and scoliosis could complicate neuraxial anesthetic techniques in parturients with Marfan syndrome. Patent Ductus Arteriosus Pregnancy is nicely tolerated in sufferers with patent ductus arteriosus, and issues are uncommon. Coarctation of the Aorta Women with repaired coarctation of the aorta tolerate pregnancy properly. The coarctation could additionally be associated with a bicuspid aortic valve in more than half the sufferers. Use of neuraxial anesthesia avoids the opposed results of myocardial despair and positivepressure air flow on the Fontan circulation, which lacks a functioning proper ventricle (see Table 41.
Effect of hemodialysis on uterine and umbilical artery Doppler move velocity waveforms anxiety 24 hours a day buy 10 mg atarax visa. Acute renal failure in pregnancy in a developing country: twenty years of expertise anxiety symptoms headaches cheap 10 mg atarax mastercard. Acute kidney injury associated to being pregnant in developing international locations: etiology and threat components in an intensive care unit anxiety symptoms similar to heart attack atarax 10 mg buy line. Investigation of an increase in obstetric acute renal failure within the United States, 1999-2011. Acute kidney damage community: report of an initiative to enhance outcomes in acute kidney damage. Incidence and outcomes of acute kidney harm in intensive care models: a Veterans Administration examine. Short-and long-term prognosis of blood strain and kidney disease in ladies with a past historical past of preeclampsia. Pregnancy in sufferers on chronic dialysis: a single middle expertise and combined evaluation of reported results. Pregnancy in dialysis patients in the new millennium: a systematic evaluate and meta-regression evaluation correlating dialysis schedules and being pregnant outcomes. The youngsters of dialysis: live-born infants from on-dialysis mothers in Italy�an epidemiological perspective evaluating dialysis, kidney transplantation and the general population. Improving hand hygiene compliance charges in the haemodialysis setting: extra than just more hand rubs. Cardiovascular despair after brachial plexus block in two diabetic sufferers with renal failure. Plasma concentrations of bupivacaine after supraclavicular brachial plexus blockade in patients with chronic renal failure. Serum protein binding of propofol in sufferers with renal failure or hepatic cirrhosis. Preoperative serum cholinesterase concentration in persistent renal failure: clinical experience of suxamethonium in 81 sufferers present process renal transplant. Acute tubular necrosis and pre-renal acute kidney damage: utility of urine microscopy of their evaluation-a systematic evaluate. Decreasing incidence of renal cortical necrosis in patients with acute renal failure in developing international locations: a single-centre expertise of twenty-two years from japanese India. Endotoxin and renal perform: perspectives to the understanding of septic acute renal failure and poisonous shock. Idiopathic postpartum renal failure: evaluation and case report of a successful renal transplantation. Postpartum hemolytic uremic syndrome: a examine of three instances with a evaluation of the literature. Early analysis and management of postpartum hemolytic uremic syndrome with plasma exchange. The long-term consequences of thrombotic microangiopathy (thrombotic thrombocytopenic purpura and hemolytic uremic syndrome) in pregnancy. Reversible acute renal failure in association with bilateral ureteral obstruction and hydronephrosis in pregnancy. Acute kidney damage during being pregnant and puerperium: a retrospective examine in a single heart. Pregnancy outcomes following maternal kidney transplantation: a national cohort study. Renal hemodynamics in normal and hypertensive pregnancy: lessons from micropuncture. Pregnancy in renal transplant recipients: long-term effect on affected person and graft survival. Low-dose computed tomography for the evaluation of flank pain within the pregnant inhabitants. The increased incidence of renal stones in ladies with spontaneous abortion: a retrospective research. The use of medical expulsive therapy during being pregnant: a worldwide perspective amongst consultants. Urolithiasis in being pregnant: current prognosis, treatment, and pregnancy issues. Pregnancy outcomes in solid organ transplant recipients with publicity to mycophenolate mofetil or sirolimus. Pregnancy in renal transplantation: immunologic analysis of neonates from moms with transplanted kidney. Biochemical screening for Down syndrome in pregnancies following renal transplantation. Darbepoetin alfa therapy for post-renal transplantation anemia throughout being pregnant. Delayed presentation of an extradural abscess complicating thoracic extradural analgesia. Stone formation and pregnancy: pathophysiological insights gained from morphoconstitutional stone evaluation. Experience with the diagnosis and management of symptomatic ureteric stones during pregnancy. Airway obstruction produces the clinical manifestations of wheezing, cough, and dyspnea. Airway irritation modulates the course of asthma by independently producing airway obstruction and enhancing airway hyperresponsiveness. Airway hyperresponsiveness is marked by exaggerated responses to all kinds of bronchoconstrictor stimuli, including histamine, methacholine, prostaglandin F2, hypoosmotic options, and chilly air. Pathophysiology Asthma is believed to happen beneath quite a lot of environmental influences within the presence of genetic susceptibility. The most essential potential mechanisms are (1) an enhancement of contractility or an impairment of leisure of airway clean muscle, (2) a neural imbalance, (3) airway inflammation, and (4) changes within the perform of the airway epithelium. Epidemiology Asthma is an more and more frequent downside amongst younger, in any other case healthy ladies of childbearing age. From 2001 to 2010, the prevalence of asthma in the United States elevated from 7. For many years, an enhancement of airway clean muscle responsiveness to contractile agonists was assumed to be a major mechanism of bronchial asthma. To check this speculation, investigators attempted to correlate airway responsiveness in vivo and in vitro in humans5�9 and in the basenji-greyhound canine model of bronchial asthma. Instead of an enhancement in responsiveness to contractile stimuli, a discount in responsiveness to relaxant stimuli may contribute to airway obstruction. One examine demonstrated impaired relaxant responses to isoproterenol in airway smooth muscle from human asthmatic subjects as compared with the responsiveness of airway easy muscle from controls. Neural Components A balance between constricting and dilating influences also exists with respect to the autonomic nervous system. A shift on this steadiness, with a rise in constricting influences, could also be a mechanism of bronchial asthma. Efferent cholinergic fibers travel in the vagus nerve to synapse in ganglia throughout the airway wall. Muscarinic autoreceptors, or receptors on the nerve ending,14 also are activated by acetylcholine and inhibit additional launch of acetylcholine from the nerve terminal. The significance of exaggerated cholinergic efferent exercise in the pathogenesis of airway hyperreactivity has been debated extensively. However, this mechanism seems to be very important within the perioperative administration of asthmatic topics. Reflex stimulation of airway easy muscle by placement of a tracheal tube represents one of the necessary causes of bronchospasm within the perioperative period. An alternative mechanism by which the parasympathetic nervous system might contribute to airway hyperresponsiveness is through dysfunction of the muscarinic autoreceptors. Dysfunction of these receptors allows increased postganglionic launch of acetylcholine after reflex stimulation. In contrast to the parasympathetic nervous system, sympathetic innervation of airway easy muscle in human subjects is both sparse or absent. The alpha-adrenergic system is believed to play a comparatively minor role in figuring out the state of airway responsiveness. Although alpha-adrenergic receptors are present in human airways,20 the protecting results of alpha-adrenergic antagonists have been disappointing and may be attributed to different properties, similar to antihistamine exercise. Afferents from the airway originate within the epithelium and are activated by airway irritation, as happens with tracheal intubation.
Pin Heads (German Chamomile). Atarax.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96914
A later potential examine of ninety six women showed that use of leukotriene receptor antagonists was not related to a particular pattern of congenital abnormalities anxiety zone atarax 25 mg generic on-line, but the investigators cautioned that extrapolation of the information to a big inhabitants would require further research due to the restricted sample size of the study anxiety symptoms one side 10 mg atarax discount with mastercard. Anesthetic Management Preoperative Assessment During the preoperative analysis anxiety psychiatrist atarax 25 mg discount otc, the anesthesia provider ought to assess the severity of the illness and whether an acute asthmatic episode is current. The medical history ought to include information about symptoms of wheezing, dyspnea, and cough. Further info must be sought about the frequency and severity of signs, the course of these signs during being pregnant, and the date of the most recent exacerbation. Chest auscultation could reveal wheezing with or without a extended expiratory part. Additional signs of an acute exacerbation of bronchial asthma embrace tachypnea, an exaggerated (greater than 20 mm Hg) pulsus paradoxus, and the use of accent respiratory muscles. In a pregnant girl with secure bronchial asthma, laboratory checks add little to anesthetic management. However, if an acute exacerbation is suspected, chest radiographic examination, arterial blood fuel measurements, and pulmonary perform exams might help with diagnosis and therapy. Chest radiographic examination helps diagnose precipitating or complicating conditions corresponding to pneumonia, pneumothorax, and heart failure. During an episode of acute bronchial asthma, arterial blood gas measurements typically present hypoxemia and respiratory alkalosis. After a chronic, extreme episode, arterial carbon dioxide tension increases because of fatigue. The most handy indirect measurement for assessing airway obstruction throughout labor is the peak expiratory flow price, which can be measured at the bedside with a Wright peak flowmeter. It is important to stop hyperpnea and stress in girls who describe asthmatic episodes triggered by exercise or stress. These goals must be accomplished with minimal sedation, minimal paralysis of the muscles of respiration, and minimal melancholy of the fetus. Possible analgesic regimens embody systemic opioids, paracervical block, pudendal nerve block, lumbar sympathetic block, and epidural or spinal analgesia utilizing native anesthetic agents, opioids, or each. Systemic opioids might provide cheap pain aid and scale back the stimulus to hyperpnea, particularly during the early part of the primary stage of labor. Opiate receptors are believed to be current in the respiratory tract94 and to Obstetric Management the next features of obstetric administration of the asthmatic parturient might differ from that of the nonasthmatic patient: (1) induction of labor, (2) management of postpartum hemorrhage, and (3) treatment of hypertension. For induction of labor, prostaglandins should be administered cautiously in women with bronchial asthma. Likewise, bronchial asthma represents a relative contraindication to the administration of 15-methyl prostaglandin F2 (carboprost, Hemabate) for the treatment of postpartum hemorrhage. The use of ergot alkaloids to deal with postpartum hemorrhage in asthmatic women has additionally been questioned. Beta-adrenergic receptor antagonists are used to deal with hypertension in some pregnant women. Paracervical block and pudendal nerve block carried out by an obstetrician are acceptable selections for analgesia in the course of the first and second stages of labor, respectively. These techniques provide analgesia without sedation or paralysis of the respiratory muscles. The problems with these strategies in asthmatic girls are similar to those in nonasthmatic parturients (see Chapter 24). Lumbar sympathetic block also provides ache reduction with out sedation or motor block during the first stage of labor. This approach has the identical limitations as for women without asthma (see Chapter 24). The advantage of the absence of motor block must be weighed towards the chance for respiratory despair in asthmatic topics. Advantages of the use of native anesthetic brokers for lumbar epidural analgesia in asthmatic patients embody steady ache relief and a reduction in the stimulus to hyperventilation. These goals sometimes are achieved with out maternal sedation or neonatal despair. Unlike different analgesic techniques, steady lumbar epidural analgesia provides a margin of security by offering the opportunity to lengthen the sensory block for cesarean delivery. The risk of extension allows the anesthesia supplier to avoid a number of the dangers related to general anesthesia. The most important drawback of epidural native anesthetics in an asthmatic subject is the chance for a high thoracic motor block and respiratory insufficiency. Use of an acceptable epidural catheter take a look at dose and upkeep of a sensory degree at the tenth thoracic dermatome minimize this risk. In addition, using a dilute concentration of local anesthetic mixed with a modest dose of an opioid produces passable analgesia with less motor block than local anesthetic alone. In basic, avoidance of airway instrumentation is desirable, because tracheal intubation markedly will increase airway tone in asthmatic topics. Neuraxial anesthesia is associated with a lower incidence of bronchospasm than common anesthesia in asthmatic topics. In unstable asthmatic patients who require using accessory muscles of respiration, neuraxial anesthesia could additionally be hazardous due to impaired ventilatory capacity within the presence of a high thoracic motor block. General anesthesia for asthmatic girls undergoing cesarean supply requires a stability between the competing issues of pulmonary aspiration and intraoperative bronchospasm. Although airway instrumentation supplies a great stimulus for bronchospasm, the high danger for aspiration mandates tracheal intubation throughout administration of common anesthesia in parturients. Most generally, choices for tracheal intubation include awake intubation and rapid-sequence induction, although mask induction of general anesthesia with sevoflurane has been described in a parturient with status asthmaticus. The benefits of topical local anesthetics and airway nerve blocks for awake intubation must be weighed in opposition to a attainable increase in the danger for aspiration from the lack of protecting airway reflexes. Rapid-sequence induction for cesarean delivery in asthmatic sufferers is most frequently completed utilizing either propofol or ketamine. A sympathomimetic agent, ketamine has long been thought-about the intravenous induction agent of alternative for asthmatic subjects. Beneficial airway results of propofol, like those of ketamine, also appear to occur by way of inhibition of airway reflexes. Intravenous lidocaine, which also inhibits airway reflexes, attenuates irritant-induced bronchoconstriction,108 together with tracheal intubation, and produces a further protecting impact above that of beta-adrenergic agonist pretreatment alone. After supply, upkeep of anesthesia sometimes consists of nitrous oxide and an intravenous opioid, with or and not using a low concentration of a risky halogenated agent. In asthmatic parturients, the unstable halogenated anesthetic brokers are considered the brokers of selection for the maintenance of anesthesia. These agents attenuate airway responsiveness via direct effects on airway clean muscle,110�112 inhibition of airway reflexes,113 and results on the epithelium. Although halothane and isoflurane are roughly equipotent bronchodilators at excessive concentrations, halothane produces higher bronchodilation at decrease concentrations116 and subsequently may be preferable for anesthesia for cesarean supply. Sevoflurane acts as a bronchodilator in massive and small airways117 and reverses airway constriction associated with tracheal intubation. Desflurane protects against a direct stimulus to the airways119 however may be less efficient towards reflex stimuli, corresponding to tracheal intubation. The potential drawback of this method is that the simplest bronchodilators. The administration of a beta-adrenergic agonist by aerosol delivers a comparatively greater dose of drug to the airways and minimizes uterine relaxation. Emergence from common anesthesia, as with induction, requires a stability between reducing the risk for aspiration and reducing the risk for bronchospasm. Extubation of the trachea when the patient is awake minimizes the danger for aspiration, however the tracheal tube could stimulate reflexes and precipitate bronchospasm because the depth of anesthesia is reduced. For refractory bronchospasm, continued mechanical ventilation in an intensive care unit may be required. The prevalence of smoking among pregnant ladies in the United States declined from 18. The main respiratory results of cigarette smoking embody alterations in small airway operate, elevated mucus secretion, and impairment of ciliary transport. Smoking also is associated with a rise in nonspecific airway reactivity, probably through epithelial injury, altered airway geometry brought on by increased mucus secretion, or upregulation of endothelin receptors. Interaction with Pregnancy Few studies have documented the respiratory results of cigarette smoking during pregnancy. Although additional studies are warranted, different respiratory effects of cigarette smoking in pregnant girls are likely to be similar to these effects in nonpregnant women. In a rodent mannequin, reductions in uterine blood circulate following inhaled nicotine were mediated by sympathetic nicotinic acetylcholine receptors.
Visceral pain during caesarean section under spinal and epidural anaesthesia with bupivacaine anxiety symptoms pain in chest atarax 25 mg purchase otc. Algorithms for the prevention of postoperative nausea and vomiting: an efficacy and effectivity simulation anxiety x blood and bone discount atarax 10 mg overnight delivery. A factorial trial of six interventions for the prevention of postoperative nausea and vomiting anxiety 2020 episodes 25 mg atarax with amex. Ondansetron versus placebo for the management of nausea and vomiting during caesarean section beneath spinal anaesthesia. Interventions for stopping nausea and vomiting in girls present process regional anaesthesia for caesarean part. Epidural ondansetron is more effective to stop postoperative pruritus and nausea than intravenous ondansetron in elective cesarean supply. Dexamethasone for the prophylaxis of postoperative nausea and vomiting related to neuraxial morphine administration: a systematic evaluation and meta-analysis. Intrathecal meperidine decreases shivering during cesarean delivery under spinal anesthesia. The effects of gentle perioperative hypothermia on blood loss and transfusion requirement. Core physique temperature and the thermoneutral zone: a longitudinal examine of normal human being pregnant. The influence of ambient working room temperature on neonatal and maternal hypothermia and associated morbidities: a randomized managed trial. Lower limb wrapping prevents hypotension, but not hypothermia or shivering, after the introduction of epidural anesthesia for cesarean supply. Oxytocin protocols throughout cesarean supply: time to acknowledge the risk/benefit ratio Oxytocin pretreatment decreases oxytocin-induced myometrial contractions in pregnant rats in a concentration-dependent however not time-dependent manner. Oxytocin pretreatment of pregnant rat myometrium reduces the efficacy of oxytocin but not of ergonovine maleate or prostaglandin F-2 alpha. A randomized, double-blinded trial of a "rule of threes" algorithm versus steady infusion of oxytocin throughout elective cesarean supply. Haemodynamic effects of repeated doses of oxytocin during caesarean supply in wholesome parturients. A prospective, double-blind, randomized comparison of prophylactic intramyometrial 15-methyl prostaglandin F2 alpha, one hundred twenty five micrograms, and intravenous oxytocin, 20 units, for the control of blood loss at elective cesarean section. Controlling refractory atonic postpartum hemorrhage with Hemabate sterile solution. Misoprostol as an adjunct to normal uterotonics for remedy of post-partum haemorrhage: a multicentre, double-blind randomised trial. Active administration of the third stage of labor with a mixture of oxytocin and misoprostol to stop postpartum hemorrhage: a randomized controlled trial. Anesthesia for interventional radiology in parturients at threat of main hemorrhage at cesarean part delivery. Prophylaxis for venous thromboembolic disease in being pregnant and the early postnatal interval. Amniotic fluid and rope plasma erythropoietin ranges in pregnancies difficult by preeclampsia, pregnancy-induced hypertension and persistent hypertension. Contamination of salvaged maternal blood by amniotic fluid and fetal purple cells during elective caesarean section. Intraoperative cell salvaged blood as a half of a blood conservation strategy in caesarean part: is fetal purple cell contamination essential Postpartum hemorrhage handled with an enormous transfusion protocol at a tertiary obstetric heart: a retrospective research. Inadequately treated pain could cause numerous undesirable physiologic and psychologic consequences in girls present process cesarean supply, together with impaired recovery, persistent and continual ache, and elevated price. Local and systemic inflammatory cytokines act to sensitize the peripheral nerves and improve ache notion. Multimodal pharmacologic and nonpharmacologic treatment for pain is the optimal strategy and should be supplied each time possible and medically indicated. Dotted lines represent pain reports from particular person topics, and solid white line is a shifting average. Choice of Opioid Factors that have an effect on the selection of opioid are pace of onset, period of action, total efficacy, and the type and frequency of unwanted effects. If unwanted effects forestall sufficient analgesia, other opioids or nonopioid adjuvants must be used. Patient preferences based on past experiences and desired analgesia also needs to be thought-about. A steady background infusion is typically averted besides in selected instances. Although the function of the lockout interval was not addressed on this study, the investigators advised that insufficient analgesia might be produced by lockout intervals which are too lengthy or demand doses which would possibly be too small. By contrast, larger doses or shorter lockout intervals might lead to more opioid-related unwanted facet effects. Additionally, it has been instructed that sufferers are discouraged by an inadequate analgesic impact or they may anticipate a delayed response. There had been no differences between groups in postoperative ache, sleep pattern, demand or delivered bolus dose per hour, opioid consumption, or recovery from surgical procedure. The use of a steady infusion resulted in six errors through the programming of the system. Three sufferers required discontinuation of the continual infusion due to important oxyhemoglobin desaturation. Analgesia could additionally be improved by a rise within the bolus dose, a shorter lockout interval, or a change of opioid. Because of the significant morbidity related to high doses of opioids, use of these drugs should invoke the appliance of algorithms for ache assessment, management, and monitoring. Therefore, when tolerated, oral administration of opioids may be the preferred route of administration. Advantages of this approach are price savings, facilitation of early mobility, and, perhaps, larger affected person satisfaction. The rationale of multimodal analgesia is the optimization of additive or synergistic effects of various modes of analgesia or drug lessons, whereas lowering the dose and minimizing the unwanted effects of particular person medication with completely different mechanisms of motion. The change forced the replacement of mixture oral opioid-acetaminophen analgesics with scheduled acetaminophen and as-needed opioids for postcesarean analgesia. All patients in their study obtained spinal anesthesia containing intrathecal morphine 0. After the change, the women acquired oral acetaminophen 650 mg each 6 h for forty eight h postoperatively with oral oxycodone administered as wanted for breakthrough ache. They are effective for perineal pain after vaginal supply and postcesarean abdominal ache; when coadministered with opioids, they produce a 30% to 50% opioid-sparing effect60,70 that may scale back opioid-related side effects. In a small study (oral ibuprofen four hundred mg each 6 hours for 24 hours), less than 1 mg of ibuprofen was excreted in breast milk in a 36-hour period. Ibuprofen is approved as a therapeutic drug for youngsters and therefore is considered appropriate with breast-feeding. Scheduled acetaminophen with as-needed opioids in comparability with as-needed acetaminophen plus opioids for post-cesarean ache administration. A randomized managed trial analyzing the effect of naproxen on analgesia in the course of the second day after cesarean delivery. Data have been analyzed using repeated measures evaluation of variance; sufferers within the acetaminophen/diclofenac group used less morphine per 4-hour interval than sufferers in the acetaminophen however not the diclofenac group. Alpha2-Adrenergic Receptor Agonists Alpha2-adrenergic receptor agonists have been used for the therapy of acute and continual pain in nonobstetric patients. Gabapentin Gabapentin is an anticonvulsant that has analgesic properties, notably in the setting of neuropathic ache. As part of a multimodal analgesic routine in patients undergoing cesarean supply, a preoperative dose of oral gabapentin 600 mg was related to lower pain scores with motion and at rest; nevertheless, the incidence of sedation was higher within the gabapentin group than in the placebo group (19% versus 0%). Gabapentin could play a task in postcesarean analgesia in sufferers with continual pain and people with opioid tolerance. Ketorolac beforehand had a "black field" warning that it was "contraindicated in nursing moms," however present suggestions are to use it with warning. Ketamine was superior to fentanyl and placebo for reducing pain scores at 90 and one hundred eighty minutes, and decreasing analgesic requirements within the first 24 hours, but not within the second 24 hours, after cesarean delivery. A 2015 systematic literature evaluate and meta-analysis included seven research of ketamine use during spinal anesthesia and five during basic anesthesia.
In the United Kingdom anxiety symptoms sweating order atarax 25 mg on-line, 54% of women who died from thromboembolic problems in 2009 to 2013 were chubby or overweight anxiety symptoms pain effective 10 mg atarax. The threat is further increased by decreased mobility anxiety 300 buy atarax 25 mg cheap, comorbidities such as preeclampsia, and an increased frequency of operative delivery. A 2014 meta-analysis reported an association between sleep-disordered breathing and low start weight, neonatal intensive care unit admission, fetal progress restriction, and a 1-minute Apgar score lower than 7. Other Comorbidities Obesity is associated with an increased risk for numerous illness states compared with lean controls (Table 49. Endocrine Changes Gestational diabetes and diabetes mellitus happen extra regularly in obese patients. Those repeated durations of hypoxemia and reoxygenation lead to important endocrine and metabolic disturbances, which end in an increased risk for hypertension, myocardial infarction, stroke, diabetes, and metabolic syndrome. The incidence of co-morbidities associated to obesity and obese: a systematic evaluation and meta-analysis. Overweight, obesity, and despair: a scientific review and meta-analysis of longitudinal studies. Obesity is associated with a significantly elevated incidence of maternal, fetal, and neonatal problems. These include a better threat for spontaneous abortion (miscarriage), thromboembolic problems, gestational diabetes, hypertensive problems of being pregnant, dysfunctional labor, shoulder dystocia, operative vaginal delivery, cesarean supply, postpartum hemorrhage, wound an infection, fetal macrosomia, fetal congenital anomalies, stillbirth, and neonatal death (Table 49. The report of Confidential Enquiries into Maternal Deaths within the United Kingdom for 2012 to 2014 confirmed that 51% of girls who died had been overweight or obese, a pattern that has been consistent for the last a quantity of reviews. The impression of obesity on maternal mortality is particularly evident in ladies who die of thromboembolism or cardiac disease. Six of the thirteen direct maternal deaths attributed to anesthesia in the United Kingdom between 2003 and 2008 occurred in overweight parturients. Possible explanations embrace elevated fetal size, higher labor induction charges, and/ or decreased responsiveness to oxytocin. Myometrium obtained from obese women at cesarean delivery contracted with less pressure and frequency and had less calcium flux than that from normal-weight women. Obesity can be related to a higher risk for failed medical induction of labor. Operative vaginal delivery, with its related maternal and fetal morbidity, is also extra likely within the overweight parturient. Obesity, obstetric complications and cesarean delivery rate-a population-based screening study. Labor and Vaginal Delivery Many of the choices for labor analgesia have limitations within the obese parturient. Further, inhalation analgesia could result in a reduced degree of consciousness, which could be very harmful in an obese lady with a troublesome airway. Neuraxial analgesia represents the most suitable choice for pain reduction and is especially desirable in the overweight parturient. Given the larger risks for fetal macrosomia and shoulder dystocia in overweight sufferers, sufficient analgesia is often wanted to facilitate an atraumatic vaginal supply. The use of epidural analgesia throughout labor allows the anesthesia provider to prolong epidural analgesia to surgical anesthesia for cesarean supply and thus keep away from the necessity for common anesthesia with its associated dangers. Given the increased chance for cesarean supply and the larger risk for common anesthesia in the overweight parturient, the early administration of neuraxial labor analgesia is beneficial in the obese parturient. When performing a neuraxial anesthetic method in the obese parturient, technical difficulties could include (1) incapability to palpate the spinous processes or identify the midline5; (2) greater depth of the epidural house,sixty one which may exaggerate minor needle directional errors and increase the likelihood of identifying a lateral portion of the epidural space62; and (3) the presence of fat pockets as well as hormonal softening of the ligaments, which may end in a false lack of resistance and/or higher danger for unintentional dural puncture. Observing the prominence of the seventh cervical vertebra and the gluteal cleft can facilitate identification of the midline. Asking the parturient in regards to the perceived location of the needle during block placement (relative to the midline) can also facilitate identification of the midline. Probing the subcutaneous tissue with a needle also can assist identify the spinous processes and assist identify a lumbar interspace. More objectively, ultrasonographic steering can be utilized to identify the midline, image the epidural house, and measure the gap from the skin to the epidural space (see Chapter 12). A variety of technical matters ought to be considered when caring for an overweight parturient. An appropriate-sized blood strain cuff have to be used for noninvasive blood strain measurements. Unless the length of the sphygmomanometer cuff exceeds the circumference of the arm by 20%, systolic and diastolic blood strain measurements may overestimate true maternal blood stress. Ultrasonographic steerage could also be helpful; nevertheless, if peripheral intravenous entry is unsuccessful, central venous cannulation could also be necessary. Appropriately sized labor beds, transportation gurneys, and working tables, and enough personnel to help with patient transport, are imperative. Although standard working tables are typically rated for individuals weighing up to 500 pounds (227 kg), this rating could additionally be inadequate for morbidly obese sufferers, especially when the desk is articulated. Special equipment for shifting and positioning the affected person, similar to motorized lifts, and longer spinal/epidural needles, may be needed (see later discussion). However, gentle tissue compression with the ultrasound probe resulted in underestimation of the depth of the epidural space in obese women. Placing the affected person in the sitting position facilitates identification of the midline and is most popular by many anesthesia suppliers when initiating a neuraxial anesthetic process in overweight parturients. In the lateral place, gravity could cause lateral fats to sag downward and obscure the midline. Further, the space from the pores and skin to the epidural area is minimized when the affected person is within the sitting-flexed position. Movement of the epidural catheter relative to the skin is most striking in overweight sufferers. The distance from the skin to the epidural area increases, and an unsecured catheter will appear to be drawn inward by as much as 1. Therefore, these investigators recommended that the patients assume the lateral position earlier than the epidural catheter is secured to the pores and skin. Alternatively, when putting the block in the sitting-flexed place, the patient should be asked to sit upright before taping the catheter to the pores and skin. Many authors have documented technical difficulties with neuraxial strategies in overweight parturients. In 1993, Hood and Dewan71 reported that 94% of sufferers who weighed more than 300 lb (136. More attempts were required to establish the epidural house in overweight girls, there was a significantly higher preliminary failure rate (42% versus 6%), and placement of a second or third epidural catheter was extra often required. Similarly, using an up-down sequential allocation research design to estimate the median efficient epidural bupivacaine dose (administered in a volume of 20 mL), Panni and Columb80 found that obese girls required significantly less epidural bupivacaine for initiation of labor analgesia than lean parturients. The targets of epidural labor analgesia ought to be the supply of excellent pain aid with minimal motor block. Epidural administration of a dilute resolution of native anesthetic with a lipophilic opioid provides analgesia for labor whereas minimizing antagonistic effects corresponding to hypotension and motor blockade. The neuroblockade offered to obese parturients in labor should be bilateral and close to perfect. Otherwise, the epidural catheter must be eliminated and replaced because an insufficient block with a frequent need for top-up doses may result in failure of extending the block for cesarean supply. In a study of morbidly obese parturients revealed in 1993, the preliminary administration of native anesthetic by way of the epidural catheter resulted in failure of analgesia/anesthesia in 42% of the ladies, a fee that was seven occasions larger than that in management parturients. In instances of unintentional dural puncture, steady spinal analgesia can be used to provide labor analgesia. In addition to providing reliable labor analgesia, continuous spinal analgesia may be transformed to spinal anesthesia for emergency cesarean supply. It is crucial, nevertheless, that the catheter be clearly labeled and all personnel are made aware of its intrathecal location. Unintentional administration of an epidural dose of local anesthetic through the spinal catheter markedly will increase the chance for high spinal block and subsequent respiratory arrest. In a retrospective examine of 516 women with unintentional dural puncture with a 17-gauge Tuohy needle, Peralta et al.
Extension of Epidural Labor Analgesia the extension of epidural labor analgesia to surgical anesthesia enough for cesarean delivery could be achieved with a number of native anesthetic brokers anxiety chest tightness cheap atarax 25 mg online. Extension of epidural analgesia may be initiated as preparations are being made to move the affected person from the labor room to the operating room anxiety from weed buy 25 mg atarax visa. Whether an in situ epidural catheter must be used for an extension attempt is decided by several elements anxiety signs 10 mg atarax order visa, together with the standard of the prevailing labor analgesia. A systematic evaluation and meta-analysis discovered that the incidence of failed conversion of labor analgesia to cesarean supply anesthesia is bigger when an rising variety of epidural boluses have been required to produce adequate labor analgesia, a larger urgency for cesarean delivery exists, and a nonobstetric anesthesiologist is managing the case. A meta-analysis of 11 randomized managed trials examining the sort of native anesthetic used to "top-up" epidural labor analgesia for emergency cesarean delivery216 in contrast 0. The pooled analysis instructed that lidocaine with epinephrine resulted within the fastest onset of sensory block; the addition of fentanyl additional hastened block onset, but not high quality as measured by the necessity for intraoperative supplementation. Compared with bupivacaine, ropivacaine was related to a decrease need for intraoperative supplementation, and lidocaine demonstrated a trend toward decrease need. The epidural administration of 2% lidocaine with freshly added epinephrine 5 �g/mL was compared with 3% 2-chloroprocaine in a randomized trial involving 40 women undergoing elective cesarean supply. However, given the time taken to prepare the lidocaine with epinephrine solution, the investigators concluded that use of a pre-prepared answer, such as 2-chloroprocaine, may be preferred. Alkalinization of the local anesthetic answer not only will increase the speed of onset but also improves the standard and prolongs the duration of neuroblockade. Although this phenomenon could be demonstrated for all local anesthetics, alkalinization is most often carried out with local anesthetic agents of brief and medium period. In a randomized trial, 40 ladies with functioning epidural labor analgesia acquired a 3-mL epidural check dose of 2% lidocaine with epinephrine, adopted by 10 8 Minutes 12 mL of premixed 2% lidocaine with epinephrine 5 �g/mL (1: 200,000) and fentanyl seventy five �g with 1. Extension of a T10 level of analgesia to a T4 level of anesthesia typically requires a volume of 15 to 20 mL of native anesthetic with one or more adjuvants. At our establishment, the extension of epidural labor analgesia begins with evaluation of the standard of analgesia. For emergency cesarean supply, we initiate the extension of epidural anesthesia in the labor room by giving 10 mL of alkalinized 2% lidocaine (with epinephrine) or 3% 2-chloroprocaine. The sensory blockade is assessed after transfer of the patient to the working room; if the blockade is bilateral and shifting in a cephalad path, a further 5 to 10 mL is administered to convey the sensory level to T4. The extension of epidural analgesia to epidural anesthesia within the labor room is controversial. However, this follow could increase the chance for failed epidural anesthesia, necessitating the induction of basic anesthesia with its attendant risks (see later discussion). Chloro, 2-chloroprocaine; Bicarb, bicarbonate; Lido, lidocaine; Epi, epinephrine 5 �g/mL. Epidural lidocaine versus 2-chloroprocaine for fetal misery requiring pressing cesarean section. In addition, basic anesthesia offers a bonus in circumstances during which uterine rest could be helpful. The fundamental elements for preparation and care of the obstetric patient present process cesarean delivery apply to the patient present process general anesthesia (Box 26. The preanesthetic analysis should focus on evaluation of physical characteristics. The consent process should characteristic the dangers associated with airway administration, aspiration, and consciousness. Administer a bolus and/or a steady infusion of oxytocin; contemplate different uterotonic agents. Perform tracheal extubation when neuromuscular blockade is fully reversed and the patient is awake and responds to commands. Send blood specimen for baseline laboratory measurements; contemplate sort and display (or cross-match) if danger factors for peripartum hemorrhage are present. Give metoclopramide 10 mg and/or ranitidine 50 mg intravenously greater than 30 minutes earlier than induction, if attainable. Perform a group "time-out" to verify affected person identity, position, and operative website; procedure to be carried out; and availability of particular gear, if wanted. Provide 100 percent oxygen with a tight-fitting face mask for three minutes or longer, when potential, for denitrogenation/preoxygenation. Otherwise, instruct the patient to take 4 to eight vital-capacity breaths instantly earlier than induction of anesthesia. After the stomach has been prepared and operative drapes are in place, confirm that the surgeon and assistant are ready to start surgery. Attempts must be made to decrease each the risk for maternal aspiration and the chance for pulmonary injury if aspiration happens. We administer metoclopramide 10 mg and ranitidine 50 mg intravenously between 30 and 60 minutes earlier than induction of general anesthesia, when attainable, to diminish gastric quantity and gastric acid secretion, respectively. If the affected person has airway traits that herald troublesome mask ventilation or intubation, consideration ought to be given to performing an awake tracheal intubation (see Chapter 29). Glossopharyngeal and laryngeal nerve blocks may be thought of, although these ought to be prevented in sufferers at excess risk for bleeding. The head, neck, and shoulders must be optimally positioned for airway administration. Preoxygenation (denitrogenation) with 100 percent oxygen must be carried out to delay the onset of hypoxemia during apnea; this hypoxemia happens more rapidly because of the pregnancy-induced lower in useful residual capability and increase in oxygen consumption. After the surgical drapes have been applied and the working personnel are prepared at the tableside, the surgeon ought to be instructed to delay the incision until the anesthesia provider confirms right placement of the endotracheal tube and gives verbal directions to proceed with surgical procedure. Induction A rapid-sequence induction is initiated with denitrogenation/ preoxygenation followed by administration of an induction agent, paralysis, and cricoid stress. Some guidelines226 have advised modification of the rapid-sequence induction to include gentle, lowpressure (Pmax 20 cm H2O) mask air flow to verify that air flow is possible and to maximize oxygen reserve whereas awaiting induction and paralysis. Whether rapid-sequence induction with or without modification ought to be employed, notably in an appropriately fasted, nonlaboring patient presenting for elective cesarean supply, has been questioned. Application of the total amount of pressure while the patient remains to be awake can provoke active retching and regurgitation. In some instances, cricoid strain could also be briefly released to allow a profitable intubation; not sometimes the good thing about launch outweighs the risk for regurgitation. Cricoid stress should then be reapplied till the right endotracheal tube place is confirmed. Historically, thiopental (4 to 6 mg/kg) has been the most incessantly used induction agent. Propofol, in a dose sufficient for induction and to forestall maternal consciousness (2. Pregnancy appears to be related to much less extreme succinylcholineinduced fasciculations and muscle pain. Some recent information recommend its use in cesarean supply may be associated with a decrease frequency of myalgia in contrast with succinylcholine. Auscultation should be carried out to rule out inadvertent endobronchial intubation. The anesthesia provider should also observe ongoing proof of adequate maternal oxyhemoglobin saturation as well as bilateral thoracic motion and breath sounds. If incorrect endotracheal tube placement is promptly acknowledged, extubation (with continued cricoid pressure) will often permit another attempt without the necessity for added muscle relaxant. Anticipation of a troublesome endotracheal intubation, or a failed intubation attempt, ought to invoke the difficult airway algorithm and a call for help (see Chapter 29). Options embrace (1) allowing the patient to awaken, (2) using various techniques to place an endotracheal tube, and (3) utilizing various airway units. Emergency airway tools must be immediately obtainable in all obstetric working rooms. However, any system that can facilitate ventilation must be used as a lifesaving device in situations of failed intubation. Maintenance the targets for anesthetic maintenance embrace (1) adequate maternal and fetal oxygenation, with maintenance of normocapnia for pregnancy; (2) applicable depth of anesthesia to promote maternal comfort and a quiescent surgical area and to stop consciousness and recall; (3) minimal effects on uterine tone after delivery; and (4) minimal antagonistic results on the neonate. These objectives may be completed utilizing inhalational anesthesia or, much less commonly, complete intravenous anesthesia. Although the use of a higher Fio2 can increase maternal arterial and umbilical venous blood oxygen content material, this motion has not been noticed to end in differences in 1- or 5-minute Apgar or neurobehavioral scores.
As a consequence anxiety in dogs symptoms atarax 25 mg cheap with amex, obstetric anesthesia providers should always give careful attention to aseptic approach anxiety explained purchase atarax 25 mg on-line, especially throughout performance of a neuraxial procedure anxiety 5 things images buy atarax 10 mg on-line. Proper sterile approach for neuraxial procedures contains sporting a face masks, performing hand hygiene, and donning sterile gloves (see Chapter 12). An increasing number of institutions are utilizing premixed options of native anesthetic and opioid (prepared under aseptic situations in a hospital or compounding pharmacy) to limit breaches in aseptic method in the course of the administration of neuraxial anesthesia. Intravenous Access and Fluid Management the institution of functional intravenous entry is of critical significance to the profitable end result of many medical conditions in obstetric anesthesia follow. Because the scale of the catheter, greater than the size of the vein, dictates the flow rate, using a brief, large-diameter catheter. Smaller catheters may be acceptable in an emergency; quantity and blood resuscitation can be satisfactorily achieved using 20- and 22-gauge catheters (without evidence of larger purple blood cell destruction) with the usage of dilution, pressurization, or each. The type of fluid (crystalloid, colloid) and the volume, price, and timing of administration are related factors in the prevention and remedy of hypotension. Traditionally, approximately 1 L of crystalloid answer has been administered intravenously (as "prehydration" or "preload") to prevent or scale back the incidence and severity of hypotension during neuraxial anesthesia for cesarean delivery. However, prehydration, even with massive volumes (30 mL/kg), is minimally effective in stopping neuraxial anesthesia-induced hypotension. For sufferers at high threat for hypotension or the consequences of hypotension, colloid may be administered before or on the time of initiation of neuraxial blockade. Supplemental Medications for Anxiety the administration of benzodiazepines, even low doses. However, every so often, particularly in women with extreme nervousness or undergoing an emergency cesarean supply, the use of low doses of intravenous midazolam or an opioid could facilitate performance of a neuraxial method, awake tracheal intubation, or the induction of basic anesthesia. The supine hypotension syndrome, which is brought on by compression of the aorta and inferior vena cava by the gravid uterus, can manifest as pallor, tachycardia, sweating, nausea, hypotension, and dizziness. Fifteen degrees of left lateral tilt (left uterine displacement) has been proposed to significantly cut back the opposed hemodynamic penalties of the supine position, though each the aorta and inferior vena cava could remain partially compressed. The editors have chosen to retain using the abbreviation �g throughout this textual content. Lateral tilt should be utilized in all ladies in mid- to late being pregnant after the administration of neuraxial or common anesthesia, with higher tilt used when possible if aortocaval compression is suspected because the cause for maternal or fetal compromise. If blankets are used to create the ramp place, they need to be stacked quite than interlaced, to enable for speedy removing and readjustment of the head and neck place if essential. The worth of this strategy in preventing hypotension throughout neuraxial anesthesia has been questioned. Whether the use of the lateral or the sitting place is best for routine initiation of neuraxial anesthesia is controversial. Theoretically, the lateral place may be of value during development of an epidural needle as a end result of it minimizes the prominence of the dural sac. Bulging of the lumbar dural sac-particularly in the sitting position-may decrease the pressure required to create a dural puncture with a Tuohy epidural needle, but this risk is unproven. The sitting place also has some advantages, including simpler landmark recognition in obese parturients and ease of positioning sufferers in a symmetrical position (the spine is commonly rotated in the lateral position as a result of the underside shoulder is fixed). It grew to become a typical apply following the seminal report by Fox and Houle100 that demonstrated improved oxygenation, better umbilical cord blood acid-base measurements, and fewer time to sustained respiration in the neonate, when mothers undergoing cesarean supply with neuraxial anesthesia breathed one hundred pc oxygen as an alternative of air for at least 10 minutes. However, later evidence suggested that routine oxygen administration could additionally be pointless, ineffective101 and probably detrimental. Nonetheless, the emergency cesarean supply of the compromised fetus should embody maternal oxygen administration of excessive Fio2, significantly within the setting of uterine contractions, which might exacerbate fetal compromise; in these situations, supplemental oxygen could scale back the severity of fetal hypoxia with restricted oxygen free-radical results. The exercise of these compensatory mechanisms and their relationship to gestational age and labor suggest that the highest threat for ischemia-reperfusion injury happens in preterm fetuses earlier than the onset of labor. Of curiosity, when asphyxiated infants are immediately resuscitated at birth with air as a substitute of one hundred pc oxygen, higher shortterm outcomes have been observed114,one hundred fifteen; this discovering may be a result of the shift in the stability between useful oxygenation and detrimental free radicals. Although the value of supplemental oxygen use throughout elective cesarean delivery with neuraxial anesthesia of a noncompromised fetus is questionable, some obstetric anesthesia suppliers place nasal cannulae or a mask to monitor air flow using expired carbon dioxide analysis. The most acceptable anesthetic method for cesarean delivery is determined by maternal, fetal, and obstetric factors (Table 26. The urgency and anticipated duration of the operation play an necessary role in the number of an anesthetic technique. A standardized four-grade classification system could additionally be used to talk the degree of urgency among providers (Table 26. Effective communication with the obstetric group is critical to set up the diploma of urgency, which helps guide selections relating to anesthetic management. Further, up to date requirements for affected person safety require that each one members of the surgical group participate in a preoperative "time-out" to verify (1) the correct patient id, position, and operative site; (2) settlement on the procedure to be carried out; and (3) the availability of special tools, if needed. In circumstances of emergency cesarean supply, the emotional needs of the mother and father are additionally necessary. Parental misery commonly occurs in this setting, and the anesthesia supplier is commonly the most effective individual to give reassurance. In modern apply, neuraxial anesthesia is administered to some sufferers who would have received common anesthesia prior to now. Umbilical wire prolapse, placenta previa, and preeclampsia with severe options are now not thought of absolute indications for basic anesthesia. For example, in some circumstances a prolapsed umbilical cord could be decompressed, and if fetal standing is reassuring, a neuraxial approach can be used. In an analysis of obstetric anesthesia trends within the United States between 1981 and 2012, a progressive improve was famous in the use of neuraxial anesthesia, especially spinal anesthesia, for each elective and emergency cesarean deliveries. Spinal anesthesia is taken into account an appropriate technique even in probably the most urgent settings; in a tertiary care institution with a median of 9500 cesarean deliveries yearly, neuraxial anesthesia was used in more than 99% of cesarean deliveries over a 6-year interval. Maternal mortality following general anesthesia has been a main motivator for the transition towards higher use of neuraxial anesthesia for cesarean supply. A research compared the anesthesia-related maternal mortality price from 1979 to 1984 with that for the interval from 1985 to 1990 within the United States. Of interest, these information might overstate the relative danger related to general anesthesia, as a result of this technique of anesthesia is used principally when neuraxial anesthetic methods are contraindicated for medical reasons or time constraints. The type of maternal morbidity differs with the use of neuraxial anesthetic techniques and common anesthesia. A systematic evaluation of randomized and quasi-randomized managed trials evaluating major maternal and neonatal outcomes with using neuraxial anesthesia and general anesthesia for cesarean delivery found much less maternal blood loss and shivering however extra nausea in the neuraxial anesthesia group. Evidence suggests that administration of prophylactic antibiotics earlier than incision (rather than after wire clamping) reduces the incidence of postcesarean endometritis and complete maternal infectious morbidity. Prospective audits of post-cesarean supply outcomes have indicated that in the first postoperative week, sufferers who received neuraxial anesthesia had less ache, gastrointestinal stasis, coughing, fever, and melancholy and were capable of breast-feed and ambulate more rapidly than sufferers who obtained general anesthesia. Apgar and neonatal neurobehavioral scores are comparatively insensitive measures of neonatal well-being, and umbilical cord blood gasoline and pH measurements might mirror the rationale for the cesarean delivery quite than differences in the effect of the anesthetic technique on fetal/neonatal well-being. In a scientific evaluate of randomized trials in which the indication for cesarean supply was not urgent, no variations in umbilical twine arterial blood pH measurements had been discovered amongst common and neuraxial anesthetic methods. With all neuraxial methods, an adequate sensory level of anesthesia is necessary to decrease maternal ache and avoid the urgent want for administration of general anesthesia. Because motor nerve fibers are sometimes larger and harder to block, the complete absence of hip flexion and ankle dorsiflexion most probably signifies that a practical sensory and sympathetic block can be present in an analogous (primarily lumbosacral) distribution. However, because afferent nerves innervating abdominal and pelvic organs accompany sympathetic fibers that ascend and descend within the sympathetic trunk (T5 to L1), a sensory block that extends rostrally from the sacral dermatomes to T4 ought to be the objective for cesarean supply anesthesia. The manner in which the level of sensory blockade is assessed has implications for the success of a neuraxial method. A potential study of 102 women present process cesarean supply with spinal anesthesia indicated that although sensory blockade to gentle contact differed from sensory blockade to pinprick or chilly sensation by 0 to eleven spinal segments, no fixed relationship among these ranges could be determined. Sensory examination ought to move caudad to cephalad in the mid-axillary line on the lower extremities but may be performed within the mid-clavicular line on the torso. The time at which an enough block is achieved, as properly as the cephalad level of the block and the presence of surgical anesthesia of the decrease abdomen, must be documented on the anesthetic document. Because the undersurface of the diaphragm (C3 to C5) and the vagus nerve could also be stimulated by surgical manipulation during cesarean delivery,129 maternal discomfort (including shoulder pain) and other signs. Neuraxial or systemic opioids assist stop or alleviate these signs (see later discussion). Given these advantages, spinal anesthesia is essentially the most commonly used anesthetic method for cesarean delivery in the developed world. A number of different needle designs can be found (see Chapter 12); the dimensions and design of the needle tip have an effect on the incidence and severity of post�dural puncture headache (see Chapter 30).