Ayurslim
Ayurslim
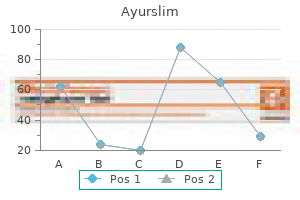
Ayurslim dosages: 60 caps
Ayurslim packs: 1 packs, 2 packs, 3 packs, 4 packs, 5 packs, 6 packs

Patients with more severe liver manifestations normally current at an older age or during adolescence herbals biz buy ayurslim 60 caps mastercard. Hepatomegaly and splenomegaly jb herbals purchase 60 caps ayurslim free shipping, secondary to portal hypertension herbs native to outland buy 60 caps ayurslim visa, are frequent physical findings. Caroli illness and Caroli syndrome: Cystic liver illness involving the big intrahepatic bile ducts. Because of bile stasis within the cysts, affected patients are predisposed to recurrent cholangitis. Ductal plate malformation, as in congenital hepatic fibrosis, can additionally be present in Caroli syndrome. Fat Hepatomegaly because of fats accumulation is seen in plenty of disorders, the most common of which are obesity, speedy weight change, diabetes mellitus, and malnutrition. Obesity in addition to fast weight achieve can lead to hepatomegaly, which is related to steatosis, delicate inflammation, and Kupffer cell hyperplasia. The presence of the metabolic syndrome (visceral weight problems, hypertension, insulin resistance/ diabetes mellitus, and dyslipidemia) appears to be more essential than weight problems alone in the development of steatosis and steatohepatitis. Ethnic background can also be a threat factor; Hispanics and Native Americans are at highest threat, and African Americans are at lowest danger. Treatment consists primarily of weight reduction and management of hyperglycemia and hyperlipidemia. Common hepatic options embody hepatomegaly (from cholesteryl ester and triglyceride accumulation), elevated serum aminotransferase ranges, progressive liver fibrosis, and cirrhosis. Progressive liver illness with steatosis, fibrosis, and cirrhosis can happen in more than half of sufferers. The illness normally presents within the neonatal interval with persistent vomiting, diarrhea, malabsorption (secondary to accumulation of lipid in the intestinal epithelium), failure to thrive, and hepatosplenomegaly. Profound hypoglycemia develops after short durations of fasting with lactic acidosis, hyperuricemia, hypophosphatemia, and hyperlipidemia. Treatment features a high-starch food regimen typically within the form of cornstarch or continuous feedings to provide a steady source of glucose. Because this kind of disease can progress to cirrhosis with hepatic failure, liver transplantation is considered an efficient remedy; however, cardiac and neurologic features have been reported to turn into obvious after transplantation. Mauriac syndrome, found in sufferers with kind 1 diabetes mellitus, is characterised by the triad of poorly managed diabetes mellitus, growth retardation, and hepatomegaly. Three types are recognized: Type I sometimes manifests with hepatosplenomegaly and is a persistent nonneuropathic form of the disease. Liver biopsy specimens are characterised by lipid-laden "foam cells" and saved sphingomyelin in macrophages. Niemann-Pick illness type C, unlike varieties A and B, outcomes from lipid-trafficking defects that causes accumulation of unesterified ldl cholesterol and sphingolipid in affected cells. The onset of neurocognitive dysfunction and visceral illness is variable however more widespread in childhood than in infancy and adulthood. Affected patients could current with neonatal cholestasis or options of liver illness later in infancy or childhood. Liver transplantation has been undertaken to deal with liver illness related to this dysfunction (see Chapter 20). Copper storage illnesses (see also Chapter 19) Wilson illness is a genetic illness brought on by copper overload; the irregular gene is situated on chromosome 13. Defective copper excretion leads to excess accumulation within the liver with subsequent accumulation in the central nervous system and other organs. Diagnosis is by a serum ceruloplasmin degree <20 mg/dL, liver copper >250 g/g dry weight, and urinary copper excretion >100 g/day. Liver biopsy specimens show steatosis early within the course; the illness progresses to irritation and fibrosis with cirrhosis. Without treatment, the disease can be progressive and deadly as a outcome of hepatic failure. D-penicillamine and trientine are chelators that improve urinary excretion of copper. Some patients current with acute liver failure; the only efficient therapy possibility on this scenario is liver transplantation, which is healing. Tumors which will infiltrate the liver secondarily embrace neuroblastoma, Wilms tumor, and lymphoma. Viral Hepatitis (see Chapters 3 to 5) Hepatitis A and hepatitis B are the most typical causes of viral hepatitis in children. Although both hepatitis A and hepatitis B could manifest as an acute febrile illness with jaundice and hepatomegaly, the courses could differ. Hepatitis A Hepatitis A virus is transmitted by the fecal-oral route, and outbreaks can typically be traced to daycare centers where hygiene could additionally be suboptimal. Adults who work with youngsters in daycare centers are at an increased risk of contracting this illness. The disease is often mildly symptomatic (75% to 95%) in kids without visible jaundice, whereas adults are more commonly symptomatic (75% to 95%). Because the disease is self-limited, no particular remedy is required, but follow-up is needed to exclude development to acute liver failure. Hepatitis A vaccination is very effective in preventing medical illness (94%) for kids and adults at excessive threat. Hepatitis B Perinatal transmission of hepatitis B virus from a highly infectious mom is a vital route of infection in endemic areas. Hepatitis C Maternal-to-infant transmission is a standard route for childhood infection, with perinatal transmission rate of 5%; intravenous drug abuse is a typical route of transmission in adolescents. In the United States, approved treatment for youngsters includes peginterferon-alfa2b together with ribavirin. In 2017, the mixture of oral direct-acting antiviral agents ledipasvir and sofosbuvir was accredited for kids aged 12 to 17 with an infection caused by genotypes 1, 4, 5, or 6. Because these agents are highly effective and fewer poisonous than interferon-based regimens, treatment may be deferred till these new brokers are accredited for kids under age 12 or different regimens are approved for kids with genotype-2 or genotype-3 infection. Patients present with hepatomegaly, which may be erroneously attributed to hyperinflation of the lungs. Sickle cell illness Patients with sickle cell illness generally have hepatomegaly, apparently secondary to sinusoidal dilatation and Kupffer cell hyperplasia. An elevated frequency of cholelithiasis secondary to fast hemoglobin turnover is seen on this population. Risk factors embody prematurity, stomach surgery, necrotizing enterocolitis, and infections, notably catheter-related bloodstream infections. Fish oils or multisource lipid emulsions as the lipid part are associated with decision of jaundice and will scale back hepatobiliary illness. Celiac disease Patients with celiac disease may current with serum aminotransferase elevations, a protracted prothrombin time, or nonspecific liver histologic modifications even within the absence of gastrointestinal symptoms. A gluten-free food regimen sometimes normalizes each laboratory and liver histologic abnormalities. A significant proportion have autoimmune options (autoimmune sclerosing cholangitis). Childhood histiocytic syndromes: Abnormal activation of the reticuloendothelial system might lead to liver illness. Abnormally activated Langerhans cells can infiltrate the liver, thereby resulting in elevated serum aminotransferase ranges, hypoalbuminemia, prolongation of the prothrombin time, and hepatomegaly. Liver histology generally demonstrates a portal tract inflammatory infiltrate composed of lymphocytes, neutrophils, and eosinophils. Patients who require liver transplantation could additionally be at elevated danger of acute mobile rejection and posttransplantation lymphoproliferative disease. This multiorgan disease is caused by abnormal activation of nonmalignant macrophages. Diagnostic standards include 5 of the next eight options: Fever, splenomegaly, cytopenia (2 cell lines): Hemoglobin <9 g/dL; platelets <100 � 109/L; neutrophils <1. Inborn errors of glycosylation: Carbohydrate-deficient glycoprotein syndromes comprise a bunch of multisystem problems with defects in N-linked oligosaccharide meeting. Patients can current in infancy with variable levels of liver dysfunction secondary to steatosis or fibrosis.
Other malformations of the cranium and facial (craniofacial) region may include downslanting eyelid folds (palpebral fissures) biotique herbals order 60 caps ayurslim otc, a flat nasal bridge herbals on express 60 caps ayurslim best, malformed (dysplastic) quality herbals products pvt ltd ayurslim 60 caps buy with mastercard, low-set ears, small dental malformations,152 and underdeveloped (hypoplastic) higher or decrease jaw (maxilla or mandible), or both. Additional abnormalities might embrace brief stature, structural heart malformations (congenital heart defects), delicate to reasonable weight problems, protrusion of parts of the intestine by way of an abnormal opening in the belly wall close to the navel (umbilical hernia), or failure of the testes to descend into the scrotum (cryptorchidism) in affected males. Both regular intellect and mild psychological retardation have been reported in patients with Carpenter syndrome. Mandibular hypoplasia is among the main anomalies of the mandible, with a profound effect on airway administration. Micrognathia leads to posterior regression of the tongue and a small hyomental space. The mandible develops from the primary branchial arch and is a function in lots of rare syndromes. Glossoptosis makes displacement of the tongue to the left troublesome, so the airway is tough to visualize. Pierre Robin sequence, which affects 1 in 8500 newborns,157 was described in 1923 by Pierre Robin as airway obstruction related to glossoptosis and hypoplasia of the mandible. At present, this syndrome is characterised by retrognathia or micrognathia, glossoptosis, and airway obstruction. Pierre Robin sequence outcomes from failure of mandibular growth through the first several weeks of embryogenesis. This causes posterior displacement of the tongue, which prevents regular growth and closure of the palate. The Pierre Robin sequence represents a spectrum of anatomic anomalies whose common features include mandibular hypoplasia, glossoptosis, and cleft palate. Four kinds of airway obstruction have been described in sufferers with Pierre Robin sequence; in only 50% is the obstruction completely related to posterior positioning of the tongue. This might clarify why the usage of an oral or nasopharyngeal airway alone may not enhance an already troublesome masks airway. Patients who fail to improve after glossopexy or nasopharyngeal airway placement, or both, usually require tracheostomy. The micrognathia causes posterior displacement of the tongue, preventing normal growth of the palate. Because of the higher airway obstruction present, an elective tracheostomy was performed. Prone posturing was efficient in the remedy of mild airway obstruction in eighty two patients (90. Treacher Collins syndrome (mandibulofacial dysostosis, Franceschetti syndrome) outcomes from a poor vascular provide to the primary visceral arch in the course of the initial three to four weeks of gestation and is believed to be brought on by a change in the gene on chromosome 5 that affects facial improvement and results in hypoplasia of the facial bones, particularly the zygoma and the mandible. There is a 50% probability that the child will pass the trait on to future generations. Facial clefting causes a hypoplastic facial appearance, with deformities of the ear, orbital, midface, and decrease jaw areas. The clinical appearance is a results of the zygoma (malar bone) failing to fuse with the maxilla, frontal, and temporal bones. Highly variant levels of involvement (complete, incomplete, abortive) could be seen, however frequent facial options embody hypoplastic cheeks, zygomatic arches, and mandible; microtia with possible hearing loss; high-arched or cleft palate; antimongoloid slant to the eyes; colobomas; elevated anterior facial peak; malocclusion (anterior open bite); small oral cavity and airway with a normalsized tongue; and pointed nasal prominence. Most children with Treacher Collins syndrome have normal growth and intelligence. Because of the small jaw and airway, combined with the traditional dimension of the tongue, respiratory problems can occur at delivery and during sleep when the base of the tongue obstructs the small hypopharynx. Rasch and coauthors176 advocate that kids with obstructive symptoms have laryngoscopy before anesthetic induction. Synonyms of Goldenhar syndrome (hemifacial microsomia) are first and second branchial arch syndrome, facioauricular vertebral spectrum, oculoauricular vertebral dysplasia, and oculoauriculovertebral spectrum disorder. The main function of this condition is unilateral underdevelopment of one ear (which could not even be present) related to underdevelopment of the jaw and cheek on the same facet of the face. There are sometimes pores and skin tags or pits in entrance of the ear or in a line between the ear and the nook of the mouth. Children with the Goldenhar finish of the spectrum may have congenital heart diseases in 5% to 58% of cases (ventricular septal defect, patent ductus arteriosus, tetralogy of Fallot, coarctation of aorta). Difficulties in airway administration end result from mandibular hypoplasia, cleft or high-arched palate, cervical vertebral anomalies, and scoliosis. Nager syndrome (mandibulofacial dysostosis) is a rare craniofacial dysfunction with fewer than one hundred cases reported in the medical literature. The morphologic options of Nager syndrome embody downslanted palpebral fissures, malar hypoplasia, a high nasal bridge, atretic exterior auditory canals, and micrognathia (severe underdevelopment of the lower jaw). Proximal limb malformations embody absent or hypoplastic thumbs, hypoplasia of the radius, and shortened humeral bones. However, sufferers with Treacher Collins syndrome have extra extreme maxillary and zygomatic hypoplasia, downslanting palpebral fissures, and lower lid coloboma. Among the additional problems of youngsters with Nager syndrome are abdomen and kidney reflux and hearing loss. Associated cleft lip or cleft palate, or both, and maxillary hypoplasia with midface deformities might further complicate airway administration and applicable mask match during masks ventilation. One patient had laryngospasm during induction, and one was intubated by an otolaryngologist. Hallermann-Streiff syndrome (oculomandibulodyscephaly with hypotrichosis or oculomandibulofacial syndrome) is uncommon, with approximately one hundred fifty instances reported. Upper airway obstruction may end result from small nares and glossoptosis secondary to micrognathia, which can lead to cor pulmonale. Small nostrils, deviated nasal septum, high-arched palate, and anterior larynx preclude blind nasotracheal intubation. The ascending ramus of the mandible is both underdeveloped or absent, leading to a small mouth cavity. Intubation was achieved with problem in two circumstances with the patient underneath inhaled anesthesia. Manifestations of the syndrome embody main amenorrhea, genital immaturity, and short stature; intelligence is usually normal. Additional related features that will affect the administration of anesthesia embody hypertension, quick neck, excessive palate, micrognathia, the occasional presence of aortic stenosis or coarctation of aorta, and an absent kidney. In another case, direct laryngoscopy demonstrated immobile vocal cords, which had been approximated to each other in the midline secondary to arthritis of the cricoarytenoid joints. Mouth and Tongue Anomalies Microstomia Microstomia (a small mouth opening) is uncommon and could also be congenital or acquired. Pediatric microstomia may be congenital (in Freeman-Sheldon [whistling face], Hallermann-Streiff, and otopalatodigital syndromes) however is extra often acquired after unintentional thermal accidents, similar to biting an electrical extension twine or ingesting family lye. The vertebrae may fail to grow, and ankylosis of the apophyseal joints might result. Difficulty in sustaining the airway patency and lack of ability to intubate the trachea are essentially the most critical anesthetic problems in these youngsters. The three primary abnormalities are microstomia with pouting lips, camptodactyly with ulnar deviation of the fingers, and talipes equinovarus. Patients may be at elevated danger for malignant hyperthermia and postoperative pulmonary problems. As discussed earlier, Hallermann-Streiff syndrome is a rare congenital dysfunction in which the presence of mandibular hypoplasia and microstomia makes intubation difficult. Again, these sufferers have brittle natal enamel that might be simply broken or avulsed during laryngoscopy. The small nostrils, deviated nasal septum, high-arched palate, and anterior larynx preclude blind nasotracheal intubation. The ascending ramus of the mandible could either be underdeveloped or absent, leading to a small mouth cavity. Even tracheostomy proved to be difficult in these instances; subsequently an experienced pediatric otolaryngologist must be available. Direct laryngoscopy may be troublesome because of rigid scar tissue, which obscures the mandibular and laryngeal anatomy, or microstomia after retraction of scar tissue in facial burns. Bilateral commissurotomy to permit insertion of the laryngoscope into the mouth can additionally be reported. Microstomia from lye ingestion may be related not solely with restricted mouth opening but also with such extreme intraoral scarring that widespread landmarks guiding both inflexible or flexible fiberoptic laryngoscopy are obscured, rendering oral and nasal intubation difficult or inconceivable.
Syndromes
Lateral cervical backbone radiography to show absence of bony displacement after intubation in a patient with an acute sort iii odontoid fracture herbs for anxiety 60 caps ayurslim effective. Performance enchancment system and postoperative corneal accidents: Incidence and threat elements herbalshopcompanycom ayurslim 60 caps generic with mastercard. Corneal harm and its protection using hydro-gel patch during common anesthesia herbs and uses buy 60 caps ayurslim otc. Skull base injury with in depth pneumocephalus after transnasal endotracheal intubation. Xylometazoline pretreatment reduces nasotracheal intubation-related epistaxis in paediatric dental surgical procedure. The Parker Flex-Tip tube for nasotracheal intubation: the influence on nasal mucosal trauma. External compression of a nasotracheal tube as a end result of the displaced bony fragments of a number of LeFort fractures. The use of a nasogastric tube to facilitate nasotracheal intubation: a randomised managed trial. Utility of typical radiography within the diagnosis and administration of pediatric airway overseas bodies. The evaluation of three strategies to verify tracheal tube placement within the emergency setting. Guided orotracheal intubation in the working room utilizing a lighted stylet [letter]. Intraoperative administration of tracheobronchial rupture after double-lumen tube intubation. The effects of thermal softening of double-lumen endobronchial tubes on postoperative sore throat, hoarseness and vocal wire injuries: a potential double-blind randomized trial. The complications of tracheal intubation: A new classification with a review of the literature. If doubtful, take it out: Obstruction of tracheal tube by prominent aortic knuckle. Respiratory and circulatory compromise related to acute hydrothorax during operative hysteroscopy. An evaluation of main errors and equipment failures in anesthesia administration: Considerations for prevention and detection. Laser safety in otolaryngology: Head and neck surgery-Anesthetic and educational considerations for laryngeal surgery. Positive end-expiratory stress lowers the danger of laser-induced polyvinyl chloride trachealtube fires. Subcutaneous cervical and facial emphysema with using the Bonfils fiberscope and high-flow oxygen insufflation. Efficacy of the transillumination methodology for acceptable tracheal tube placement in young children: a randomized controlled trial. Submandibular approach for tracheal intubation in sufferers with panfacial fractures. Case history quantity 89: A life-threatening complication of cricothyroid membrane puncture. Injury to terminal branches of the trigeminal nerve following tracheal intubation. Retrograde endotracheal intubation: an underutilized device for administration of the tough airway. Percutaneous transtracheal air flow for anesthesia: A review and report of problems. Ventilation with the Ventrain via a small lumen catheter in the failed paediatric airway: two case reviews. The efficacy of three totally different modes of transtracheal air flow in hypoxic hypercarbic swine. Balloon dilatational tracheostomy: Initial expertise with the Ciaglia Blue Dolphin technique. Percutaneous tracheostomy: A 6 yr potential evaluation of the single tapered dilator technique. Hemodynamic and catecholamine stress responses to insertion of the Combitube, laryngeal mask airway or tracheal intubation. The haemodynamic response to the insertion of the laryngeal masks airway: A comparability with laryngoscopy and tracheal intubation. Differences in cardiovascular response to airway stimulation at completely different websites and blockade of the responses by lidocaine. Emergent management of the airway: New pharmacology and management of comorbidities in cardiac illness, ischemia and valvular coronary heart disease. Fiberoptic intubation using a brand new adapter, laryngeal masks insertion, or conventional laryngoscopic intubation. The efficacy of lidocaine to forestall laryngospasm in youngsters: a systematic review and metaanalysis. Pulmonary mechanics throughout basic anesthesia: the influence of mechanical irritation on the airway. A survey of perioperative bronchospasm in 105 patients with reactive airway disease. Analyses of 1500 laryngeal masks makes use of by one anaesthetist in adults present process routine anaesthesia. Prevention of endotracheal tube-induced coughing during emergence from basic anesthesia. The incidence of aspiration associated with the laryngeal masks airway: A meta-analysis of revealed literature. Intra-ocular pressure changes associated with intubation with the intubating laryngeal masks airway in contrast with typical laryngoscopy. Intraocular pressure extra lowered during anesthesia with propofol than with sevoflurane: both combined with remifentanil. Sufentanil or clonidine for blunting the increase in intraocular strain throughout rapid-sequence induction. In sufferers with head injury undergoing rapid sequence intubation, does pretreatment with intravenous lignocaine/lidocaine lead to an improved neurological end result Effects of fiberoptic bronchoscopy on intracranial pressure in sufferers with mind damage: A prospective scientific examine. Decrease within the fee of sensitization and scientific allergy to pure rubber latex. Multi-centre retrospective analysis of anaphylaxis during basic anaesthesia within the United Kingdom: aetiology and diagnostic efficiency of acute serum tryptase. Prevalence of latex allergy amongst anesthesiologists: Identification of sensitized but asymptomatic individuals. Cross-reactions in the latex-fruit syndrome: A relevant role of chitinases but not of complex asparagine-linked glycans. Blood pressure and pulserate responses to endotracheal extubation with and with out prior injection of lidocaine. Response of left ventricular ejection fraction to restoration from general anesthesia: Measurement by gated radionuclide angiography. Effects of landiolol, a short-acting beta-1 blocker, on hemodynamic variables during emergence from anesthesia and tracheal extubation in elderly sufferers with and with out hypertension. Local airway anesthesia attenuates hemodynamic responses to intubation and extubation in hypertensive surgical patients. Efficacy of endotracheal lidocaine administration with steady infusion of remifentanil for attenuating tube-induced coughing during emergence from complete intravenous anesthesia. Laryngospasm throughout anaesthesia: A computer-aided incidence study in 136,929 sufferers. Tracheal extubation of deeply anesthetized pediatric patients: A comparability of desflurane and sevoflurane. Tracheomalacia because of brief time period ventilation after total hip arthroplasty in an adult with long standing goiter. Circulatory collapse after pneumonectomy (an uncommon complication from using a Carlens catheter). Difficult extubation as a result of transfixation of a nasotracheal tube by a Kirschner wire. Displacement of the endotracheal tube brought on by change of head place in pediatric anesthesia: Evaluation by fiberoptic bronchoscopy. A prospective examine of unplanned endotracheal extubation in intensive care unit patients.
Spontaneous Ventilation and Insufflation Techniques Open techniques can be utilized throughout anesthesia for laser procedures on the vocal cords herbals 2015 60 caps ayurslim purchase amex, with spontaneous air flow strategies being utilized in adults and in kids herbals a to z purchase ayurslim 60 caps mastercard. Spontaneous ventilation and insufflation strategies are useful in the elimination of foreign our bodies herbs native to outland generic ayurslim 60 caps fast delivery, evaluation of airway dynamics. The technique requires a spontaneously breathing affected person and offers a clear view of an unobstructed glottis. Insufflation of anesthetic gases and agents could be achieved by several routes: a small catheter introduced into the nasopharynx and placed immediately above the laryngeal opening; a tracheal tube cut short and positioned by way of the nasopharynx, rising simply past the soft palate; a nasopharyngeal airway; and the facet arm or channel of a laryngoscope or bronchoscope. However, great care should be taken to stop the catheter or nasopharyngeal airway from getting very near or coming into the larynx. This would offer a fuel source that might easily cause an airway hearth if struck by a laser beam. If the catheter is inadvertently inserted too far, it could enter the esophagus, causing marked gastric distention and possible regurgitation. At a suitable depth of anesthesia, as assessed by clinical observations of the rate and depth of respiration, pupil dimension, eye reflexes, blood stress, and heart fee changes, laryngoscopy is undertaken and topical lidocaine administered Anesthesia Management for Laryngeal Laser Surgery Many laryngeal lesions are resected and eliminated with assistance from a laser, together with papillomas, vocal cord cysts, vocal wire polyps, Reinke edema, vocal twine granulomas, vocal wire microwebs, and scar tissue after intubation. The preoperative assessment ought to establish the sort and measurement of laryngeal lesion to establish the extent of airway compromise and establish the overall medical standing of the patient. The exact anesthesia technique chosen is decided by the experience of the anesthesiologist, surgical desire and access, gear obtainable, kind of laser used, period of the procedure, kind and vascularity of the lesion, and safety against airway soiling from blood and secretions. Two approaches are used: closed techniques, in which a cuffed laser tracheal tube is used, and open techniques, during which a cuffed laser tracheal tube is absent. One hundred % oxygen is administered by face masks with spontaneous air flow and anesthesia continued with inhalational (insufflation) or an intravenous route (propofol infusion). At an acceptable depth of anesthesia assessed by scientific observations, the surgeon undertakes rigid laryngoscopy or bronchoscopy. Movements of the vocal cords are often minimal with a spontaneously respiration approach, provided an sufficient degree of anesthesia is maintained. If the depth of anesthesia is just too light, the vocal cords might transfer, the patient might cough, or laryngospasm could occur. If the depth of anesthesia is too great, the affected person may turn into apneic with cardiovascular instability. Careful statement throughout the process, observing movements, respiratory rate and depth, cardiovascular stability, and unobstructed respiratory, is important, with the concentration of the risky anesthetic adjusted accordingly. The insufflation technique requires shut cooperation between the anesthesiologist and the surgeon. The limitations of spontaneous air flow or insufflation methods embrace the shortage of control over air flow and the potential for airway soiling. Insufflation methods will not be appropriate for giant, delicate, floppy lesions, significantly within the supraglottic or glottis areas, which can hinder the airway after the onset of basic anesthesia with spontaneous ventilation. Rita and associates concluded that although the insufflation technique is potentially hazardous, if it is accomplished accurately, it provides an appropriate anesthetic method for surgical procedure on the larynx of infants. A suspension laryngoscope and microscope, which offered glorious visualization of the larynx, had been used in these circumstances so that endotracheal intubation could be readily achieved with out moving the laryngoscope. The apneic technique removes all the flammable materials from the larynx during laser actuation and is assumed to greatly decrease the chance of an airway hearth. Weisberger and Miner acknowledged that the apneic period should be shortened for babies because of their decreased useful residual capacity. Jet Ventilation Techniques Jet ventilation methods are suitable for ventilation throughout laser surgery of most adult vocal wire lesions. The main limitation for their use is the experience of the anesthesiologist and the absence of appropriate gear. Jet ventilation strategies involve the intermittent administration of high-pressure jets of air, oxygen, or oxygen-air mixtures that entrain room air and decrease the delivered pressures. The risk of life-threatening barotrauma is the most critical complication, and it happens when entrainment of room air is absent. The frequency of air flow and the placement of the jet cannula must be chosen in accordance with the diploma of airway obstruction and the situation of the lesion. Specially designed catheters, laryngoscopes, bronchoscopes, and ventilators are available for the clinician to choose from. Many techniques have been described, claiming completely different benefits over the other strategies. Selection have to be carried out based mostly on a thorough understanding of the pathophysiology of airway obstruction and particular person expertise with use of these devices. If mucosal disruption is noticed, the jetting catheter ought to be positioned away from the mucosal opening because stress drops quickly with the space from the jetting orifice. During a 2-year period, fifty one procedures have been carried out by the investigators on 9 patients who had juvenile laryngeal papillomatosis. After induction of common anesthesia, the patients had been paralyzed with atracurium or vecuronium and anesthesia maintained with halothane or enflurane in 100% oxygen. This resulted in a speedy rise in the oxygen saturation in order that repeated extubations and surgery could continue. The median number of apneic episodes required for each process was two, with a variety of 1 to five. Supraglottic jet air flow strategies permit a clear, unobstructed view for the surgeon with no threat of a laser airway hearth. Subglottic Jet Ventilation Elective transtracheal catheter placement under local anesthesia in people with significant airway pathology or underneath general anesthesia for elective laryngeal surgical procedure has been described. Other potential problems embody blockage, kinking, infection, bleeding, and failure to site the catheter. None of the commercially available transtracheal catheters is particularly designed for laser use, and transtracheal jet air flow methods for endoscopic laser surgery of the larynx require a cautious analysis of the potential dangers and advantages. Jet Ventilation Frequency Low-Frequency Jet Ventilation Subglottic jet ventilation involves inserting a small (2- to 3-mm external diameter) catheter or particularly designed tubes. This means a gasoline source is current within the airway, and care should be taken throughout laser airway surgical procedure. Many of the subglottic catheters which are commercially obtainable have some laser-resistant properties, but when their tolerance is exceeded, the catheters can degrade and fracture. If after a fracture of the catheter and after a laser strike, jet ventilation is resumed, the distal fragment could also be forced into the distal airways. Subglottic jet air flow is more environment friendly than supraglottic jet air flow and leads to lowered driving pressures, minimal vocal cord actions, a good surgical subject, and no time constraints for the surgeon in the placement of the rigid laryngoscope. Low-frequency air flow typically describes ventilatory charges of less than 60 breaths per minute (1 Hz), and in follow, most lowfrequency ventilation is achieved by a guide Sanders-type gadget at charges of 15 to 25 breaths per minute. With enough driving pressures, this results in near-normal tidal volumes, seen chest inflation, and passive chest deflation. The green basket of the Hunsaker catheter reduces catheter tip movement within the trachea. To prevent barotrauma, a reducing valve and a pressure regulator ought to be in line in order that the oxygen pressure is proscribed to 50 psi for adults. The anesthesiologist should begin with much decrease values and steadily increase the pressure while observing the chest movements. Holding down the handheld lever controls the length and frequency of the jet of oxygen. The precise delivered tidal volume, focus of oxygen, and inspiratory pressures depend upon the quantity of air entrainment by the jet, length of the cannula and its alignment to the trachea, dimension of the laryngoscope, and lung compliance. These factors are exhausting to measure in a medical situation with any great precision and are at finest estimates. The minimal potential stress that may present enough air flow ought to be used. The Venturi jet have to be kept in perfect alignment with the trachea to achieve streaming of the flow into the lungs. Anesthesiologists should be watchful after any readjustment of the operating laryngoscope to which the jet is clamped, which can impair ventilation of the lungs. Oxygen saturation should be constantly monitored and chest motion frequently noticed. Short-acting muscle relaxants are used to stop actions of the patient that might be harmful throughout a laser operation. Gastric distention with potential regurgitation might occur with a misaligned cannula,139 and a nasogastric tube could also be required. Adequate fluids are given intraoperatively, and gases could also be humidified within the postoperative interval to forestall mucosal drying.
The aim is to quickly reduce the FiO2 to the target PaO2 and SpO2 to restrict the results of supplemental oxygen jeevan herbals hair oil 60 caps ayurslim order with mastercard. In most patients herbals on york generic ayurslim 60 caps amex, a target PaO2 of 60 mm Hg and SpO2 of 90% meets oxygenation requirements herbals shoppe hedgehog products ayurslim 60 caps purchase on-line. However, some patients might have higher PaO2 targets primarily based on their underlying cardiopulmonary status. Pressure set off sensitivity usually is set between -1 and -3 cm H2O, and a breath is triggered when a unfavorable inspiratory effort is bigger than the set sensitivity. A flow-triggered breath is delivered when the return move is less than the delivered flow. The breaths are initiated by the ventilator at the set time, as decided by the set respiratory fee, and it delivers the breath on the prescribed circulate rate until the specified tidal quantity has been achieved, after which the ventilator cycles off for passive exhalation. High peak flow charges enhance peak airway pressures and decrease imply airway pressures, which can decrease oxygenation. All three modes have uses throughout the spectrum of stabilization of ventilation, maintenance of ventilation, and weaning from mechanical assist. Patients in whom the usage of respiratory muscles is desired are often those being weaned from mechanical air flow or present process evaluation of muscle energy and adequacy of spontaneous work of respiration. Flow Pattern Modern mechanical ventilators can deliver various inspiratory move patterns. In this pattern, inspiratory flow stays fixed till the specified tidal volume is delivered, which is held till expiration. The sinusoidal wave pattern is characterized by gradually growing and reducing inspiratory circulate all through the respiratory cycle. In the decelerating ramp wave (or sawtooth wave) pattern, the move price begins maximally and reduces till the top of inspiration. It is commonly utilized in sufferers expected to be passive, as in routine use within the working room for basic anesthesia and in comatose patients. When the change reaches the trigger threshold, the ventilator delivers the predetermined tidal quantity. Peak inspiratory airway pressure and plateau pressure are variable in this setting. This increasing stress could be measured as the peak inspiratory stress, the mean airway strain, or the plateau strain, all of which try and describe the pressures that are transmitted through the airways at different levels and at different factors in the respiratory cycle. As the ventilator delivers a breath, the inspiratory flow continues until the maximum strain or allotted time is reached, and the flow then ceases. However, any change in lung compliance or airway impedance results in a change in tidal volume. The ventilator provides a breath at a low strain after which calculates the peak stress essential to ship the set tidal volume; that strain degree is delivered in the course of the next breath. This permits breath-to-breath correction and enables elevated airway pressure control. Many fashionable anesthesia machines incorporate similar ventilation modes because of this. The inspiratory stress is delivered until the move decreases to a predetermined level (usually 25% of peak flow). Increasing the inspiratory time increases imply airway pressure without growing the inspiratory plateau pressure, which can enhance oxygenation. T High, Number of seconds spent at the higher pressure; T Low, variety of seconds spent on the lower stress. Tlow often is longer in bi-level ventilation, which allows extra spontaneous breaths to occur at this strain level. Paw, Airway strain; P High, higher stress used for respiration on bi-level. The capability to preserve high mean airway pressures and decrease plateau pressures can improve oxygenation. In a 1984 publication, Chang described five mechanisms of oxygen delivery by high-frequency oscillation: direct alveolar air flow of proximal airways; bulk convective gas mixing in conductive airways by recirculation of air among neighboring airways in several cycles of opening and shutting of the alveolus; convective transport of gases; longitudinal dispersion by airway turbulence; and molecular diffusion. High-frequency ventilation is positive-pressure air flow with tidal volumes close to the anatomic useless house and respiratory charges larger than 60 breaths per minute. The imply airway strain is about by manipulation of the inspiratory move fee and an expiratory backpressure valve. Because the oscillator is uncomfortable for sufferers, elevated sedation and often a need for neuromuscular blockade is required. Careful titration of inspiratory strain and frequency are wanted to get hold of optimal settings. An initial pressure of 35 kilos per square inch is set with a fee of a hundred to one hundred fifty breaths per minute and an inspiratory fraction of 30%. Examples of direct injury are pneumonia, gastric fluid aspiration, and inhalation injury; oblique causes of damage embrace severe sepsis, shock, pancreatitis, blood product transfusion, and narcotic overdose. Namely, a scarcity of explicit standards in defining acute onset of the process, the sensitivity of the PaO2/FiO2 ratio to completely different ventilator settings, poor reliability of chest radiograph criteria, and difficulties in distinguishing purely noncardiogenic pulmonary edema from hydrostatic edema. These distinctions correlate with variations in mortality in addition to interventions that are delineated between ranges of severity. Weaning From Mechanical Ventilation the process of weaning from mechanical ventilation is a continuum from reducing support provided by the ventilator to evaluation of readiness utilizing a number of variables and eventual discontinuation of mechanical air flow. In 2001, a collective task drive from the American College of Chest Physicians, the American Association of Respiratory Care, and the American College of Critical Care Medicine examined the issue of discontinuation of mechanical ventilation and outlined patients who required prolonged mechanical air flow and techniques to liberate them from the mechanical ventilator. They found that mechanically ventilated patients spend roughly 42% of their ventilator time present process the weaning course of. The task pressure provided 12 suggestions to standardize practice for discontinuing mechanical air flow. These embody trying to find causes of respiratory failure; early discontinuation of sedation of postoperative patients; guaranteeing daily spontaneous respiration trials for patients who meet the criteria for hemodynamic, pulmonary, and mental stability; outlining standards for evaluation of sufferers on a spontaneous breathing trial; and strategies for prolonged weaning and day by day spontaneous breathing trials assisted by nonphysician practitioners inside the health care organization. The medical standards outlined by the duty pressure embrace clinically improving reason for respiratory failure, enough oxygenation (defined as PaO2/FiO2 > a hundred and fifty mm Hg or oxyhemoglobin saturation greater than 90% while receiving FiO2 0. The variety of ventilator-free days is the mean variety of days from day 1 to day 28 throughout which the patient had been breathing with out assistance for no much less than forty eight consecutive hours. In the study, the nurse and respiratory therapist assessed sufferers every day, and if preset guidelines had been met, sufferers underwent a 2-hour spontaneous respiratory trial. If the affected person handed the trial, the doctor was notified, and the affected person was extubated. The study demonstrated a decrease in ventilator days, a decrease in the variety of problems including reintubation, and lower hospital value. The task pressure also addressed the use of noninvasive ventilation and extended ventilator dependence. Complications of Mechanical Ventilation Mechanical Complications Mechanical air flow could produce complications from use of a synthetic airway and problems of using positive-pressure air flow. Because of the heterogeneous nature of the lung, even decrease volumes could also be disproportionally delivered to open alveoli. Mechanical complications of positivepressure mechanical ventilation embrace barotrauma from high airway pressures, volutrauma from massive distending volumes, and atelectrauma from ventilation at low volumes. High minute air flow from high tidal volumes or excessive respiratory rates is a typical cause. Efficacy and security of a paired sedation and ventilator weaning protocol for mechanically ventilated sufferers in intensive care [Awakening and Breathing Controlled trial]: a randomised controlled trial. Increased plateau pressures can be transmitted to the intrathoracic vessels and result in an overestimation of the central venous pressures and the pulmonary artery occlusion pressure (Table 46. Graphs of flow versus time will show initiation of a model new breath earlier than the expiration reaches zero circulate. The breath-hold allows the stress in the proximal airways to equilibrate with alveolar pressure. Management of the underlying situation is necessary, especially for patients with obstructive lung illnesses treated with bronchodilators, steroids, and antimicrobial therapies. The open lung concept of mechanical ventilation: the role of recruitment and stabilization.
Several months after extended tracheal intubation herbals outperform antibiotics in treatment of lyme disease ayurslim 60 caps without a prescription, tracheal stenosis and fibrosis could happen herbals and there uses ayurslim 60 caps sale. This normally represents the end stage of a progression from tracheal wall erosion to cartilaginous weakening to therapeutic with fibrosis herbals are us buy ayurslim 60 caps with amex. Symptoms include a nonproductive cough, dyspnea, and indicators of respiratory obstruction. However, surgical correction could additionally be needed after the tracheal lumen has been lowered to 4 to 5 mm. High-flow insufflation strategies by which small catheters are used distal to the larynx are most frequently associated with barotrauma. When air leaks into the peribronchial tissues, it could traverse into the subcutaneous space, the lung interstitium, or the pleural and pericardial cavities. Pneumomediastinum or pressure pneumothorax and possibly cardiac tamponade are the results, and chest tubes may be needed. Progressive accumulation of air may cause loss of pulmonary compliance and lack of ventilatory volume; if the accumulation is large sufficient, cardiopulmonary compromise and impossible air flow might end result. Safety mechanisms ought to be in place to prevent high-pressure airflow within the event that intrapulmonary pressures become extreme. For diseased pulmonary tissue, the bottom potential airway pressure ought to be used to forestall parenchymal blowout. Attempting to hyperextend the neck of those sufferers might lead to cervical fractures and quadriplegia. If immediate intubation is important, patients with acute cervical spine fractures may be rigorously intubated with handbook in-line stabilization, whereby the head is protected against extreme movement by a second individual. A range-of-motion check and an evaluation of neck extension should be performed earlier than inducing anesthesia. It is taken into account the safest technique for airway management in sufferers with cervical backbone injury. Prevention consists of vigilance on the a half of the practitioner and utility of adhesive tape over closed eyelids. Particularly throughout head and neck surgery, the eyelids should be taped closed, and the eyes must be lined rigorously with delicate eyepads. Treatment consists of allowing the injured eye to relaxation by use of an eye patch and making use of an antibiotic ointment. Temporomandibular Joint Injuries coagulopathies are thought-about contraindications to nasotracheal intubation. Nasotracheal intubation could additionally be problematic in the presence of hypertrophic turbinates, excessive deviation of the nasal septum, prominences on the nasal septum, chronic infections within the nasal cavity, and nasal polyposis. Minor bruising occurs in 54% of nasal intubations and most commonly involves the mucosa overlying the inferior turbinate and the adjoining septum. In case of injury to the pyriform sinus, the internal branch of the superior laryngeal nerve, the soft tissue of the pharynx, the larynx, and the superior laryngeal vessels may be broken. Patients with an obstructed nasal passage caused by convoluted turbinates are at elevated threat for this complication. Wrapping the tube with foam materials at the level of the nasal alar and cautious consideration in instances of long-term intubation might reduce or avoid this complication. Even within the absence of gross trauma, mechanical damage to the superficial epithelial layers brought on by nasal intubation results in mucociliary slowing in 65% of patients and bacteremia in one other 5. Opening the mouth is a combination of rotary and translational movement in the joint. The rotary movement permits solely a mouth opening of about 25 mm; maximal opening is achieved by the translational movement. Pathologic modifications corresponding to bone cysts, rheumatoid arthritis, and atrophy of the mandible as a result of age can scale back joint mobility and should result in fractures. The use of a nasogastric tube as a information to facilitate tracheal tube passage was found to scale back the incidence and severity of epistaxis, to enhance navigability and to require fewer manipulations than the standard technique. A closed claims evaluation of antagonistic anesthesia occasions reported that 18% of respiratory-related claims involved esophageal intubation. End-tidal capnography is crucial in confirming endotracheal placement of the tube. Other indicators, similar to equal bilateral breath sounds, symmetric bilateral chest wall motion, epigastric auscultation and statement, and tube condensation, are probably misleading. This helps to determine the proper orifice for intubation and protects the trachea from regurgitated abdomen contents. Once endotracheal intubation is achieved after an esophageal intubation, the abdomen ought to be suctioned to decrease vomiting, gastric perforation, or compromise of air flow. Perforation happens mostly over the cricopharyngeus muscle on the posterior esophageal wall, the place the esophagus is slim and skinny. Subcutaneous emphysema, pneumothorax, fever, cellulitis, cyanosis, throat ache, mediastinitis, empyema, pericarditis, and death can happen. Early detection and therapy of the situation are critical as a outcome of the mortality fee of mediastinitis is greater than 50%. An esophageal perforation must be suspected in any patient with a fever, sore throat, and subcutaneous emphysema after a troublesome intubation. A case report recognized a traumatic tracheal perforation through the esophagus in a affected person with a tough intubation. Small children, identified for placing small objects into their orifices, discover the nostrils one of the accessible websites. More than 80% of patients who aspirated a overseas body have been children, and most have been between 1 and 3 years old. Smith and colleagues reported a rhinolith that was dislodged throughout nasotracheal intubation;230 the mass had fashioned across the rubber tire of a toy automotive that the patient had positioned in his nostril 30 years earlier. If a nasal foreign physique is known or suspected, it should be gently dislodged, advanced into the oropharynx, and retrieved before intubation. Esophageal intubation is more common among inexperienced practitioners, but it might also occur in the arms of experienced clinicians. Recognition of this error have to be Bronchial intubation is common and generally tough to determine. Asymmetric chest expansion, unilateral absence of breath sounds (especially on the left side), and eventual arterial blood gas abnormalities are diagnostic options. Bronchial intubation (preferentially right-sided) is extra widespread in newborns and children, because of the small distance between the carina and the glottis. If bronchial intubation goes undetected, it may lead to atelectasis, hypoxia, and pulmonary edema. Maintenance of the Endotracheal Tube Airway Obstruction A patent airway is an absolute requirement for safe anesthesia. Airway obstruction ought to be thought of when an intubated patient has diminished breath sounds related to growing peak inspiratory pressures. Inspiratory gases must be humidified throughout lengthy anesthetics to prevent tube obstruction from dried secretions. In two patients, full airway obstruction occurred secondary to achalasia and esophageal dilation. One affected person had malignant ascites that, when mixed with a pneumoperitoneum, led to a speedy accumulation of pleural fluid with respiratory and cardiovascular compromise. This was identified as the most typical critical incident in a study of anesthesia-related human errors and gear Mean tube Movement in cm 1. The mean tube motion between flexion and extension is one third to one fourth of the length of a normal grownup trachea (12 � three cm). When inadvertent bronchial intubation is found, the tube must be withdrawn a quantity of centimeters and the lungs inflated sufficiently to broaden any atelectatic areas. In cases of persistent atelectasis, bronchoscopy may be required to remove mucous plugs. The tip of the tube should ideally be at least 2 cm above the carina, which can be approximated at the sternal angle (of Louis) adjoining to the junction of the sternum with the second rib. Appropriate orotracheal tube depths are approximately 21 cm from the teeth in adult women and 23 cm in grownup men, and nasotracheal tube depths are approximately 25 cm in ladies and 27 cm in men from the naris. However, if the ventilator continues to perform normally, the physician may be unaware of the character of the problem.
Linum (Flaxseed). Ayurslim.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96952
Other causes of transient loss of consciousness need to herbals himalaya purchase ayurslim 60 caps amex be distinguished from syncope; these include seizures herbals plant actions discount 60 caps ayurslim otc, vertebrobasilar ischemia jeevan herbals hair oil generic 60 caps ayurslim, hypoxemia, and hypoglycemia. A syncopal prodrome (presyncope) is widespread, although lack of consciousness could happen with none warning signs. Typical presyncopal signs embody dizziness, lightheadedness or faintness, weak point, fatigue, and visible and auditory disturbances. The causes of syncope can be divided into three general classes: (1) neurally mediated syncope (also known as reflex or vasovagal syncope), (2) orthostatic hypotension, and (3) cardiac syncope. Neurally mediated syncope comprises a heterogeneous group of useful disorders which are characterised by a transient change in the reflexes answerable for maintaining cardiovascular homeostasis. Episodic vasodilation (or lack of vasoconstrictor tone) and bradycardia occur in various mixtures, leading to momentary failure of blood strain management. In contrast, in patients with orthostatic hypotension due to autonomic failure, these cardiovascular homeostatic reflexes are chronically impaired. Cardiac syncope could additionally be due to arrhythmias or structural cardiac ailments that cause a lower in cardiac output. The scientific features, underlying pathophysiologic mechanisms, therapeutic interventions, and prognoses differ markedly amongst these three causes. Syncope has a lifetime cumulative incidence of up to 35% in the common population. The peak incidence within the younger happens between ages 10 and 30 years, with a median peak round 15 years. In population-based research, neurally mediated syncope is the most typical cause of syncope. Cardiovascular disease due to structural illness or arrhythmias is the subsequent most typical cause in most collection, significantly in emergency room settings and in older patients. Orthostatic hypotension additionally increases in prevalence with age because of the decreased baroreflex responsiveness, decreased cardiac compliance, and attenuation of the vestibulosympathetic reflex associated with aging. In the elderly, orthostatic hypotension is considerably more common in institutionalized (54�68%) than community-dwelling (6%) individuals, an statement most likely defined by the larger prevalence of predisposing neurologic problems, physiologic impairment, and vasoactive medication use among institutionalized patients. The prognosis after a single syncopal occasion for all age teams is generally benign. In specific, syncope of noncardiac and unexplained origin in youthful people has an excellent prognosis; life expectancy is unaffected. By distinction, syncope due to a cardiac cause, either structural coronary heart illness or major arrhythmic disease, is associated with an increased danger of sudden cardiac death and mortality from different causes. Similarly, mortality price is increased in people with syncope due to orthostatic hypotension associated to age and the related comorbid situations (Table 18-1). The upright posture imposes a unique physiologic stress upon people; most, though not all, syncopal episodes occur from a standing position. There is a lower in venous 123 return to the guts and lowered ventricular filling that result in diminished cardiac output and blood stress. The reflex increases peripheral resistance, venous return to the heart, and cardiac output and thus limits the fall in blood strain. If this response fails, as is the case chronically in orthostatic hypotension and transiently in neurally mediated syncope, cerebral hypoperfusion occurs. Syncope is a consequence of worldwide cerebral hypoperfusion and thus represents a failure of cerebral blood flow autoregulatory mechanisms. Myogenic components, native metabolites, and to a lesser extent autonomic neurovascular control are answerable for the autoregulation of cerebral blood flow (Chap. Typically cerebral blood flow ranges from 50 to 60 mL/min per 100 g mind tissue and remains comparatively constant over perfusion pressures starting from 50 to a hundred and fifty mmHg. Cessation of blood move for 6�8 s will end in loss of consciousness, while impairment of consciousness ensues when blood move decreases to 25 mL/min per a hundred g mind tissue. From the medical standpoint, a fall in systemic systolic blood pressure to ~50 mmHg or decrease will lead to syncope. A decrease in cardiac output and/or systemic vascular resistance-the determinants of blood pressure-thus underlies the pathophysiology of syncope. Common causes of impaired cardiac output embody decreased efficient circulating blood volume; increased thoracic pressure; large pulmonary embolus; cardiac brady- and tachyarrhythmias; valvular heart illness; and myocardial dysfunction. Systemic vascular resistance could also be decreased by central and peripheral autonomic nervous system diseases, sympatholytic medications, and transiently throughout neurally mediated syncope. Increased cerebral vascular resistance, most incessantly because of hypocarbia induced by hyperventilation, may also contribute to the pathophysiology of syncope. A second pattern, the "slow pattern," is characterised by growing and decreasing slow wave exercise solely. There is a sudden, transient change in autonomic efferent activity with elevated parasympathetic outflow, plus sympathoinhibition (the vasodepressor response), resulting in bradycardia, vasodilation, and/or reduced vasoconstrictor tone. In order to elicit neurally mediated syncope, a functioning autonomic nervous system is necessary, in distinction to syncope ensuing from autonomic failure (discussed below). Multiple triggers of the afferent limb of the reflex arc can lead to neurally mediated syncope. Often, nevertheless, the trigger is less simply recognized and the trigger is multifactorial. A decrease in arterial stress unloads the baroreceptors-the terminals of afferent fibers of the glossopharyngeal and vagus nerves- that are situated within the carotid sinus and aortic arch. In response to a sustained fall in blood pressure, vasopressin release is mediated by projections from the A1 noradrenergic cell group within the ventrolateral medulla. Vasovagal syncope (the widespread faint) is provoked by intense emotion, pain, and/or orthostatic stress, whereas the situational reflex syncopes have particular localized stimuli that provoke the reflex vasodilation and bradycardia that results in syncope. The underlying mechanisms have been identified and pathophysiology delineated for many of these situational reflex syncopes. The afferent trigger might originate within the pulmonary system, gastrointestinal system, urogenital system, coronary heart, and carotid artery (Table 18-2). Hyperventilation resulting in hypocarbia and cerebral vasoconstriction, and raised intrathoracic pressure that impairs venous return to the guts, play a central position in most of the situational reflex syncopes. The afferent pathway of the reflex arc differs amongst these problems, but the efferent response via the vagus and sympathetic pathways is similar. Alternately, neurally mediated syncope could also be subdivided based mostly on the predominant efferent pathway. Vasodepressor syncope describes syncope predominantly because of efferent, sympathetic, vasoconstrictor failure; cardioinhibitory syncope describes syncope predominantly related to bradycardia or asystole due to increased vagal outflow; and blended syncope describes syncope by which there are each vagal and sympathetic reflex adjustments. Postictal confusion is also rare, although visual and auditory hallucinations and close to dying and out-of-body experiences are typically reported. These embrace diaphoresis, pallor, palpitations, nausea, hyperventilation, and yawning. During the syncopal event, proximal and distal myoclonus (typically arrhythmic Neurally Mediated Syncope Reassurance, avoidance of provocative stimuli, and plasma volume growth with fluid and salt are the cornerstones of the administration of neurally mediated syncope. By maintaining stress in the autoregulatory zone, these maneuvers avoid or delay the onset of syncope. Possible exceptions are older patients (>40 years) in whom syncope is associated with asystole or severe bradycardia and sufferers with outstanding cardioinhibition because of carotid sinus syndrome. In these patients, dual-chamber pacing could additionally be helpful although this continues to be an area of uncertainty. Noninvasive beat-to-beat blood stress and heart price are shown >5 min (from 60 to 360 s) of an upright tilt on a tilt desk. Cardiac Syncope Arrhythmias Sinus node dysfunction Atrioventricular dysfunction Supraventricular tachycardias Ventricular tachycardias Inherited channelopathies Cardiac structural illness Valvular disease Myocardial ischemia Obstructive and different cardiomyopathies Atrial myxoma Pericardial effusions and tamponade a Hyperventilation for ~1 min, followed by sudden chest compression. A variant of orthostatic hypotension is "delayed" orthostatic hypotension, which happens past three min of standing; this will reflect a mild or early type of sympathetic adrenergic dysfunction. Characteristic signs of orthostatic hypotension include light-headedness, dizziness, and presyncope (near-faintness) occurring in response to sudden postural change. However, signs could also be absent or nonspecific, corresponding to generalized weak spot, fatigue, cognitive slowing, leg buckling, or headache. Neck pain, usually within the suboccipital, posterior cervical, and shoulder area (the "coat-hanger headache"), most likely as a end result of neck muscle ischemia, will be the solely symptom. Patients might report orthostatic dyspnea (thought to replicate ventilation-perfusion mismatch due to inadequate perfusion of ventilated lung apices) or angina (attributed to impaired myocardial perfusion even with regular coronary arteries).
Both approaches are facilitated by way of a medicine diary maintained in the course of the month or two before cessation; this helps to establish the scope of the issue herbs used for medicine ayurslim 60 caps on-line. Once the affected person has substantially lowered analgesic use jeevan herbals ayurslim 60 caps online buy cheap, a preventive treatment should be introduced herbals in india generic 60 caps ayurslim fast delivery, although another equally broadly used method is to begin the preventive simultaneously the analgesic discount is started. The most common reason for unresponsiveness to therapy is the utilization of a preventive when analgesics proceed to be used regularly. For some sufferers, discontinuing analgesics is very difficult; typically one of the best approach is to inform the affected person that some extent of ache is inevitable throughout this preliminary period. Management of Medication Overuse: Inpatients Some sufferers would require hospitalization for detoxing. Such patients have sometimes failed efforts at outpatient withdrawal or have a significant medical condition, corresponding to diabetes mellitus or epilepsy, which would complicate withdrawal as an outpatient. Following admission to the hospital, acute drugs are withdrawn fully on the first day, in the absence of a contraindication. On bodily examination, the eye is commonly red with a exhausting and fast, moderately dilated pupil. In combination, this group presents appreciable incapacity and is thus specifically dealt with here. Population-based estimates suggest that about 4% of adults have day by day or near-daily headache. This can typically be a challenge where the underlying trigger triggers a worsening of a major headache. For patients with primary headaches, prognosis of the headache sort will information remedy. The headache usually begins abruptly, however onset could additionally be extra gradual; evolution over three days has been proposed because the upper restrict for this syndrome. The first precedence is to distinguish between a major and a secondary reason for this syndrome. Subarachnoid hemorrhage is probably the most severe of the secondary causes and have to be excluded both by historical past or acceptable investigation (Chap. Recumbency normally improves the headache within minutes, and it can take solely minutes to an hour for the pain to return when the patient resumes an upright place. As time passes from the index occasion, the postural nature could turn into much less apparent; circumstances in which the index event occurred a number of years earlier than the eventual prognosis have been acknowledged. A putting sample of diffuse meningeal enhancement is so typical that in the appropriate clinical context the diagnosis is established. In patients with intractable headache, oral theophylline is a useful different; nevertheless, its impact is less speedy than caffeine. The diagnosis is comparatively simple when papilledema is current, but the chance should be thought of even in patients with out funduscopic adjustments. Headache on rising in the morning or nocturnal headache can be characteristic of obstructive sleep apnea or poorly managed hypertension. Initial therapy is with acetazolamide (250�500 mg bid); the headache may improve inside weeks. If ineffective, topiramate is the next treatment of selection; it has many actions that might be useful on this setting, together with carbonic anhydrase inhibition, weight loss, and neuronal membrane stabilization, likely mediated through effects on phosphorylation pathways. Posttraumatic Headache A traumatic occasion can trigger a headache process that lasts for many months or years after the event. The time period trauma is used here in a really broad sense: headache can develop following an injury to the head, but it could also develop after an infectious episode, typically viral meningitis, a flulike illness, or a parasitic infection. Symptoms may remit after several weeks or persist for months and even years after the damage. Posttraumatic headache may also be seen after carotid dissection and subarachnoid hemorrhage and after intracranial surgery. The underlying theme appears to be that a traumatic event involving the pain-producing meninges can trigger a headache course of that lasts for a number of years. Tricyclic antidepressants, notably amitriptyline, and anticonvulsants, similar to topiramate, valproate, and gabapentin, have been used with reported benefit. The monoamine oxidase inhibitor phenelzine can also be helpful in carefully chosen patients. In a practical sense, the brink for referral can also be decided by the experience of the primary care doctor in headache drugs and the supply of secondary care options. Headache Classification Committee of the International Headache Society: the International Classification of Headache Disorders, 3rd ed. The task of the primary care doctor is to determine the only a few worrisome secondary complications from the very nice majority of major and less troublesome secondary complications (Table 13-2). Absent any warning signs, a reasonable method is to treat when a analysis is established. As a basic rule, the investigation ought to focus on figuring out worrisome causes of headache or on gaining confidence if no primary headache diagnosis may be made. After remedy has been initiated, follow-up care is crucial to establish whether progress has been made against the headache grievance. Not all complications will reply to therapy, but, generally, worrisome complications will progress and shall be easier to establish. The intervertebral disks are composed of a central gelatinous nucleus pulposus surrounded by a tricky cartilaginous ring, the annulus fibrosis. Desiccation of the nucleus pulposus and degeneration of the annulus fibrosus enhance with age, resulting in loss of disk top. The disks are largest within the cervical and lumbar areas where actions of the spine are best. The anterior backbone absorbs the shock of bodily actions such as walking and running and, with the posterior backbone, protects the spinal wire and nerve roots within the spinal canal. Each arch consists of paired cylindrical pedicles anteriorly and paired lamina posteriorly. The vertebral arch also offers rise to two transverse processes laterally, one spinous process posteriorly, plus two superior and two inferior articular sides. The posterior spine supplies an anchor for the attachment of muscle tissue and ligaments. The contraction of muscles hooked up to the spinous and transverse processes and lamina works like a system of pulleys and levers that ends in flexion, extension, and lateral bending movements of the backbone. The nerve roots exit at a level above their respective vertebral bodies in the cervical region. By distinction, because the spinal twine ends at the vertebral L1 or L2 degree, the lumbar nerve roots observe a protracted intraspinal course and could be injured anywhere from the upper lumbar spine to the intervertebral foramen or extraforaminal area. Neuroimaging of the spine should embrace both sagittal and axial views to assess potential compression in both the lateral recess or intervertebral foramen. Beginning at the C3 level, each cervical (and the first thoracic) vertebral body initiatives a lateral bony course of upward-the uncinate process. The uncinate course of articulates with the cervical vertebral body above through the uncovertebral joint. The uncovertebral joint can hypertrophy with age and contribute to neural foraminal narrowing and radiculopathy within the cervical spine. Pain-sensitive constructions of the spine include the periosteum of the vertebrae, dura, facet joints, annulus fibrosus of the intervertebral disk, epidural veins and arteries, and the longitudinal ligaments. Disease of those numerous structures might explain many circumstances of back ache without nerve root compression. Attention is also focused on identification of threat elements for a severe underlying etiology. The most frequent critical causes of back ache are radiculopathy, fracture, tumor, infection, or referred pain from visceral structures (Table 14-1). Local ache is attributable to injury to pain-sensitive structures that compress or irritate sensory nerve endings. The ache is normally described as primarily stomach or pelvic, accompanied by back ache and usually unaffected by posture. Pain of backbone origin may be located in the again or referred to the buttocks or legs. Diseases affecting the upper lumbar backbone are inclined to refer ache to the lumbar area, groin, or anterior thighs. Diseases affecting the decrease lumbar backbone tend to produce pain referred to the buttocks, posterior thighs, calves, or toes. Referred ache can explain pain syndromes that cross a number of dermatomes without proof of nerve or nerve root damage.

Ultrasonography Sensitivity of 75% to 80% Findings � Complex mass filling the gallbladder lumen � Asymmetric gallbladder wall thickening � Polypoid gallbladder mass � Gallbladder wall invasion � Gallstones � Normal in as a lot as herbs collinsville il 60 caps ayurslim with visa 10% of sufferers b greenwood herbals buy ayurslim 60 caps lowest price. The typical cholangiographic appearance is an extended stricture of the midportion of the bile duct usually below the hepatic duct bifurcation herbs good for anxiety 60 caps ayurslim discount free shipping. Endoscopic or percutaneous stents could be positioned for preoperative biliary decompression, to help in surgical management, or to present long-term palliation. Biopsy for tissue diagnosis ought to only be performed in sufferers with unresectable or metastatic gallbladder most cancers. Bile duct or bile cytologic specimens or brushings, even with a cytogenetics assay. Obstructive jaundice may be palliated with either a Silastic or metallic endoprosthesis or internal-external transhepatic Silastic stent; inner or internal-external Silastic stents should be changed at 2- to 3-month intervals. Palliative systemic chemotherapy (gemcitabine plus cisplatin) may be thought of for patients with preserved efficiency status and a life expectancy >6 months. Incidental discovery of gallbladder carcinoma at laparoscopic cholecystectomy With the widespread use of laparoscopic cholecystectomy for symptomatic gallstones, many gallbladder cancers are first encountered on this setting. Laparoscopic cholecystectomy is contraindicated if gallbladder carcinoma is suspected preoperatively. If gallbladder carcinoma is recognized at the time of laparoscopic cholecystectomy, the operation ought to be transformed to an open resection. If gallbladder carcinoma is recognized pathologically after laparoscopic cholecystectomy, administration is dictated by the histologic findings. Surgical administration of suspected gallbladder carcinoma primarily based on clinical or imaging findings the resectability charges for gallbladder carcinoma range from 15% to 30%. If the tumor is confined to the lamina propria or muscular layer (pathologic stage T1), simple cholecystectomy is adequate resection in most cases. Japanese investigators have advocated more aggressive resection, together with combined hepatic resection and pancreatoduodenectomy. Postoperative morbidity and mortality charges are directly related to the extent of resection (Table 36. Adjuvant chemotherapy following resection A high frequency of distant recurrence helps the necessity for systemic adjuvant therapy. Treatment of unresectable disease Modern chemotherapy (gemcitabine and platinum-based agents) is associated with response rates of roughly 20% and improves progression-free survival by eight weeks. Because of the late stage of presentation, the general 5-year survival price is <10%, with a 2. Patients with stage I tumors have a 5-year survival fee approaching one hundred pc following sim- median survival of 6 months. The reported frequency of cholangiocarcinoma in patients with cystic abnormalities of the b. Patients with cystic lesions of the bile duct tend to develop cholangiocarcinoma at an age c. In more than 75% of patients with cholangiocarcinomas related to choledochal cysts, d. Factors that may account for the event of cholangiocarcinoma in sufferers with biliary tract ranges from 6% to 30%. The adult trematode resides within the intrahepatic and, less commonly, extrahepatic bile ducts, can hinder biliary flow, and might cause periductal fibrosis, hyperplasia, stricture, and stone formation. Hepatolithiasis (recurrent pyogenic cholangitis) (see also Chapter 35) Cholangiocarcinoma develops in 5% to 10% of patients with hepatolithiasis. Bile stasis, bactibilia, and cystic dilatation might all be associated with this elevated threat. Primary sclerosing cholangitis (see additionally Chapter 17) Average age at diagnosis: 45 to 50 years Unrecognized cholangiocarcinoma is present in as much as 25% of autopsies in patients dying with, and 15% of sufferers present process liver transplantation for, primary sclerosing cholangitis. Patients with major sclerosing cholangitis have a lifetime danger of cholangiocarcinoma of 6% to 36%. Cholangiocarcinoma in patients with major sclerosing cholangitis usually presents with fast medical deterioration and progressive jaundice. Controversy exists relating to the relation between the length of main sclerosing cholangitis and the chance of cholangiocarcinoma. The prognosis in patients with clinically detected cholangiocarcinoma and primary sclerosing cholangitis is poor, with a median survival of <1 12 months. Ulcerative colitis the frequency of cholangiocarcinoma in sufferers with ulcerative colitis ranges from 0. Cholangiocarcinoma develops 20 years earlier in sufferers with ulcerative colitis than in others. Patients with cholangiocarcinoma and ulcerative colitis tend to have pancolonic involvement and an extended period of illness. Thorotrast (thorium dioxide) this radiocontrast agent used earlier than 1960 emits alpha particles and, when injected intravenously, is retained within the reticuloendothelial system for life. Fields the province of drugs is to preserve and restore health and to relieve suffering. The perform of the ache sensory system is to defend the physique and preserve homeostasis. It does this by detecting, localizing, and figuring out potential or actual tissue-damaging processes. Sensitization occurs on the stage of the peripheral nerve terminal (peripheral sensitization) in addition to at the degree of the dorsal horn of the spinal wire (central sensitization). The cell bodies of primary sensory afferents are located nals and lower their threshold for activation by mechanical, thermal, within the dorsal root ganglia inside the vertebral foramina. Central sensitization occurs when activity, generated by nociceptors throughout irritation, enhances the excitability of nerve Dorsal root cells within the dorsal horn of the spinal cord. SensiSpinal wire tization is a clinically necessary process that contributes to tenderness, soreness, and hyperalgesia (increased pain depth in response to the identical noxious stimulus;. Sympathetic Sensitization is of explicit imporSympathetic preganglionic tance for ache and tenderness in deep postganglionic tissues. There are two distinct practical classes of axons: thermal stimuli, although hole viscera main afferents with cell bodies within the dorsal root ganglion and sympathetic postganglionic fibers with cell bodies do generate vital discomfort when within the sympathetic ganglion. Primary afferents embody these with large-diameter myelinated (A), small-diameter myelinated (A), and unmyelinated (C) axons. In contrast, when affected by Pain is an unpleasant sensation localized to part of the physique. Furthermore, any ache of reasonable or greater depth is accompanied by anxiousness and the urge to escape or terminate the feeling. Primary afferents are categorized by their diameter, diploma of myelination, and conduction velocity. These fibers are present in nerves to the pores and skin and to deep somatic and visceral structures. The ability to detect painful stimuli is totally abolished when conduction in A and C fiber axons is blocked. Individual major afferent nociceptors can reply to several different sorts of noxious stimuli. Sensitization When intense, repeated, or extended stimuli are 66 a illness process with an inflammatory element, deep constructions such as joints or hole viscera characteristically turn out to be exquisitely delicate to mechanical stimulation. A giant proportion of A and C fiber afferents innervating viscera are completely insensitive in normal noninjured, noninflamed tissue. However, in the presence of inflammatory mediators, these afferents turn out to be delicate to mechanical stimuli. Such afferents have been termed silent nociceptors, and their attribute properties might explain how, beneath pathologic conditions, the relatively insensitive deep buildings can turn out to be the source of severe and debilitating ache and tenderness. Substance P is released from primary afferent nociceptors and has multiple biologic activities. It is a potent vasodilator, causes mast cell degranulation, is a chemoattractant for leukocytes, and will increase the production and launch of inflammatory mediators. Interestingly, depletion of substance P from joints reduces the severity of experimental arthritis. The terminals of main afferent axons contact spinal neurons that transmit the ache signal to brain sites involved in pain perception. When major afferents are activated by noxious stimuli, they release neurotransmitters from their terminals that excite the spinal wire neurons. The major neurotransmitter released is glutamate, which quickly excites the second-order dorsal horn neurons. Primary afferent nociceptor terminals additionally launch peptides, together with substance P and calcitonin gene-related peptide, which produce a slower and longer-lasting excitation of the dorsal horn neurons.
Patients with head damage are in danger from this enhance because it reduces cerebral perfusion and may enhance the chance of secondary brain harm herbals india chennai discount 60 caps ayurslim free shipping. Vomiting yam herbals mysore 60 caps ayurslim discount otc, Regurgitation herbs good for hair discount 60 caps ayurslim visa, and Aspiration the general incidence of aspiration throughout common anesthesia has been reported to range from 1 in 2131 procedures (in Sweden) to 1 in 14,one hundred fifty procedures (in France). The incidence in the United States was 1 in 3216 procedures with an related mortality price of 1 in 71,829 instances. Type I hypersensitivity symptoms are localized contact urticaria with pruritus and edema. Generalized reactions embody rash or hives, tearing, rhinitis, hoarseness, dyspnea, nausea, vomiting, bronchospasm, abdominal cramping, and diarrhea. All anesthesiology departments should have a special latexsafe cart with all medical provides and devices. Although most patients tolerate these hemodynamic responses well, sufferers with cardiac disease,325 pregnancy-induced hypertension,366 and elevated intracranial stress could additionally be at specific threat for life-threatening ischemic myocardial episodes. Patients with cardiac disease have had decreased ejection fractions at the time of extubation. Pharmacologic strategies emphasize the significance of reducing the heart price, corresponding to with short-acting -blockers. During intubation, the affected person is extra protected by the induction of anesthesia induction, so hemodynamic responses could additionally be even more exaggerated during extubation. Decreased consciousness with central respiratory depression, decreased muscle tone, and tongue collapse to the posterior pharyngeal wall might lead to inspiratory or expiratory stridor, dyspnea, cyanosis, tachycardia, hypertension, agitation, and sweating. Laryngospasm can be possible, and pressing treatment is important to prevent hypoxia, mind harm, and demise. The high quality of tracheal intubation contributes to laryngeal morbidity, and wonderful intubating situations are less frequently related to postoperative hoarseness and vocal wire sequelae. Laryngospasm In a research of 136,929 sufferers, the incidence of laryngospasm was 50 circumstances per 1000 youngsters with bronchial bronchial asthma or airway infection and 25 instances per one thousand in kids 1 to 3 months old after tracheal intubation had been carried out. A patient present process deep extubation ought to be placed in the lateral position with the head down to maintain the vocal cords away from secretions throughout emergence. A examine confirmed that kids could probably be safely extubated beneath deep anesthesia with 1. This situation has numerous causes and could be classified as supraglottic, retroarytenoidal, or subglottic. Subglottic edema occurs most frequently in kids, significantly neonates and infants. Laryngeal edema usually manifests as stridor inside 30 to 60 minutes after extubation, though it may start as late as 6 hours after extubation. Regardless of the cause for laryngeal edema, management is dependent upon the severity of the condition. The apply of administering parenteral steroids with the objective of stopping or reducing edema after long-term (>36 hours) ventilation could show useful for adult sufferers, but routine administration for anesthesia is controversial. Increased left ventricular preload and afterload, altered pulmonary vascular resistance, elevated adrenergic state, proper ventricle dilation, intraventricular septum shift to the left, left ventricular diastolic dysfunction, elevated left coronary heart loading circumstances, enhanced microvascular intramural hydrostatic pressure, adverse pleural stress, and transmission to the lung interstitium could end in a marked increase in transmural pressure, fluid filtration into the lung, and growth of pulmonary edema. Management entails removing the obstruction, supporting the patient with oxygen, monitoring the patient closely, and lowering the afterload. Aspiration Pulmonary aspiration of gastric contents is a constant menace for any patient who has a full abdomen or is in danger for postoperative vomiting. Depression of reflexes, along with the presence of residual anesthetic brokers, locations most lately extubated sufferers in danger. Reducing gastric contents by suctioning through a gastric tube and extubation with the affected person positioned in the lateral position with a head-down tilt are the safest protections against aspiration. Perioperative issues in minor cases, in the event that they do occur, are usually attributed to factors such as atelectasis. Arytenoid cartilage dislocation has been reported after troublesome and routine intubations. If laryngotracheal trauma is suspected, an otolaryngology session is warranted. Airway Compression External compression of the airway after extubation might result in obstruction. This may occur after certain operations, such as carotid endarterectomy, and must be rapidly diagnosed and handled earlier than total airway obstruction happens. To minimize airway distortion, common anesthesia must be averted until the wound is evacuated beneath native anesthesia. However, even after surgical drainage, airway obstruction could happen because of venous or lymphatic congestion. The use of muscle relaxants during anesthetic induction in these patients could lead to disaster, regardless of whether the wound was beforehand drained. External compression of the neck, such as from chronic compression from a goiter, may also end result from tracheomalacia. Negative-Pressure Pulmonary Edema When airway obstruction happens after extubation within the case of laryngospasm, negative-pressure pulmonary edema could happen in a spontaneously breathing patient. As a results of inspiratory effort against a closed glottis, sufferers can generate a negative intrapleural pressure of more than one hundred cm H2O. Errors of omission embrace failure to acknowledge the magnitude of a problem, make applicable observations, and act in a well timed method. Inadequate monitoring, nonfunctional gear, and untrained workers can contribute to airway catastrophes. Airway obstruction can happen at any time during administration of common anesthesia, significantly in prolonged operations or in patients with predisposing anatomic abnormalities. The most serious complication after extubation is the prevalence of acute airway obstruction. Possible causes are failure to deflate the cuff, use of an outsized tube,384 adhesion of the tube to the tracheal wall,385 or transfixation of the tube by an inadvertent suture to a close-by organ, a wire, a screw positioned in an oromaxillofacial operation, or a damaged drill. Lingual nerve harm related to the ProSeal laryngeal mask airway: A case report and evaluate of the literature. Conclusion Anesthesiologists face many challenges and problems when managing airways. By learning from the errors of the previous, we will avoid or reduce them by anticipating issues, devising safe main and backup plans for every affected person, maintaining vigilance all through all operative procedures, and utilizing widespread sense at all times. A quantitative review and meta-analysis of efficiency of non-standard laryngoscopes and rigid fibreoptic intubation aids. The Sixth Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom. Mortality associated to anaesthesia in France: Analysis of deaths related to airway problems. Major incidents and complications in otherwise healthy patients present process elective procedures: results based on 1. Perioperative cardiac arrest: a study of fifty three,718 anaesthetics over 9 yr from a Brazilian educating hospital. Charuluxananan S, Chinachoti T, Pulnitiporn A, Klanarong S, Rodanant O, Tanudsintum S. Predictors of survival following cardiac arrest in patients present process noncardiac surgery: a examine of 518,294 patients at a tertiary referral middle. The diagnostic value of the upper lip chunk test combined with sternomental distance, thyromental distance, and interincisor distance for prediction of straightforward laryngoscopy and intubation: A potential research. The simplified predictive intubation issue score: A new weighted score for troublesome airway assessment. Comparison of five methods in predicting difficult laryngoscopy: Neck circumference, neck circumference to thyromental distance ratio, the ratio of top to thyromental distance, higher lip bite test and Mallampati test. Neck circumference as a predictor of inauspicious intubation and difficult mask ventilation in morbidly obese patients: A prospective observational research. General anaesthesia with laryngeal mask airway might cause recurrence of pneumocephalus in a affected person with head injury. Recurred pneumocephalus in a head trauma patient following positive pressure masks air flow during induction of anesthesia. Comparison of the anesthetic requirement for tolerance of laryngeal mask airway and endotracheal tube. Use of manometry for laryngeal mask airway reduces postoperative pharyngolaryngeal adverse events: A prospective, randomized trial.